Reed nevi (RNs) are almost exclusively junctional neoplasms distinguished as a variant of Spitz nevus (SN) by their significant melanogenesis and growth pattern. Acral presentation of SN is rare and has specific clinical and histopathological features.1 Nonetheless, dermoscopic findings of SN and its variants on the acral skin are poorly documented.2 Herein we describe a case of RN on the volar skin of a finger in which parallel ridge pattern was observed by dermoscopic examination.
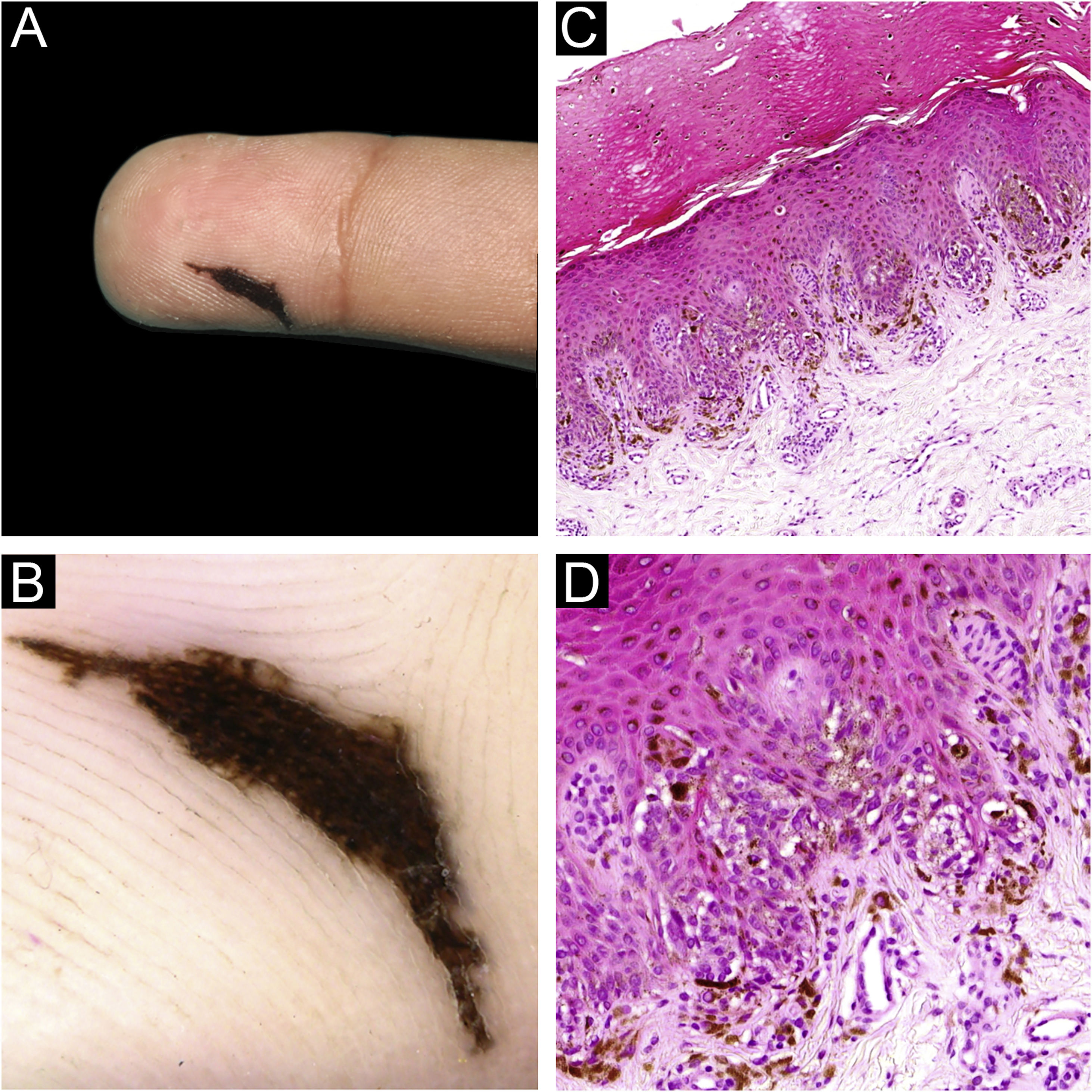
A 9-year-old boy presented with an asymptomatic pigmented lesion on his right hand. He had detected the lesion 8 months previously and had enlarged gradually. He had no personal or family history of malignant tumors. Physical examination revealed an asymmetrical dark brown macule, 13×3 mm in size, located on the volar region of the second right finger. The lesion exhibited an atypical linear morphology similar to a crescent moon (Fig. 1A). Dermoscopic findings showed a brownish parallel ridge pattern with some streaks at the periphery (Fig. 1B). A complete surgical excision was done to rule out malignancy. Histological examination revealed several small nests, vertically oriented, composed of heavily pigmented spindled melanocytes along the dermo-epidermal junction (Fig. 1C‒D). No melanocytes were seen in the dermis. A diagnosis by an RN was done.
Reed nevus on the finger (A) Clinical features of the lesion. (B) Dermoscopic findings show a parallel ridge pattern with some peripheral streaks. (C) Histopathological findings were tumor cell nests scattered within the epidermis (Hematoxylin & eosin, ×100). (D) Junctional nests were composed of heavily pigmented spindle-shaped melanocytes, vertically oriented (Hematoxylin & eosin, ×200).
Acral SNs understood by those located on soles, palms and fingers are infrequent, being reported to comprise less than 2% of all SNs.1 They are more common in young female adults, more frequently located on the feet, and larger than acral melanocytic nevi.1 Acral RN or “pigmented spindle-cell nevus” is the most common variant of SN that typically presents as a heavily pigmented lesion.1 Given the overlapping clinicopathologic features with malignancy, their clinical diagnosis is often of an atypical nevus or a malignant melanoma.1,2 Dermoscopic examination is useful in differentiating RN and acral lentiginous malignant melanoma.2 Dermoscopic patterns most commonly associated with SN are starburst and globular patterns.2 However, a characteristic pattern upon dermoscopic examination of SN localized on the glabrous skin has not been described.2,3 A review of the literature revealed only nine cases of acral SN and its variants with the dermoscopic examination.4 A parallel furrow pattern with peripheral dots, streaks, and projections and a starburst pattern has been reported in four and three cases, respectively.4 A crista-dotted pattern was described in one case of SN on the palm.3 Only Jurakić et al. in 2018 reported a young female with a rapidly growing plantar pigmented SN that had a dermoscopic parallel ridge pattern with few peripheral globules, similar to our case.5
In conclusion, we report a case of an acral RN showing a parallel ridge pattern on dermoscopy, an exception to the rule of malignancy. The present report aims to highlight that, although such a pattern is highly suggestive of melanoma, it can also be seen in a proportion of acral SNs localized on the glabrous skin. However, an SN with asymmetry and/or atypical dermoscopic pattern is impossible to differentiate from melanoma and, thereby, must be excised irrespective of age or clinical morphology.
Financial supportNone declared.
Authors’ contributionsElena Canal-Garcia: Study concept and design; drafting and editing of the manuscript; writing of the manuscript or critical review of important intellectual content; data collection, analysis and interpretation; effective participation in the research guidance; intellectual participation in the propaedeutic and/or therapeutic conduct of the studied cases; critical review of the literature; final approval of the final version of the manuscript.
Xavier Soria: Study concept and design; drafting and editing of the manuscript; writing of the manuscript or critical review of important intellectual content; data collection, analysis and interpretation; effective participation in the research guidance; intellectual participation in the propaedeutic and/or therapeutic conduct of the studied cases; critical review of the literature; final approval of the final version of the manuscript.
Felip Vilardell: Writing of the manuscript or critical review of important intellectual content; data collection, analysis and interpretation; effective participation in the research guidance; intellectual participation in the propaedeutic and/or therapeutic conduct of the studied cases; critical review of the literature; final approval of the final version of the manuscript.
Rosa M. Martí: Study concept and design; drafting and editing of the manuscript; writing of the manuscript or critical review of important intellectual content; data collection, analysis and interpretation; effective participation in the research guidance; intellectual participation in the propaedeutic and/or therapeutic conduct of the studied cases; critical review of the literature; final approval of the final version of the manuscript.
Conflicts of interestNone declared.
Study conducted at the Department of Dermatology, Arnau de Vilanova University Hospital, Lleida, Spain.