We present a different and rare manifestation of Darier’s disease, namely linear Darier’s disease. Only a few cases have been described in the literature. The case report is a male patient, 60 years old, presenting brown to red papules and plaques with hyperkeratosis distributed on the abdomen, following Blaschko’s lines, with 6 years’ evolution. It was a difficult diagnosis until the dermatological workup and biopsy.
A 60-year-old man presented for evaluation of recurrent keratotic brownish papules and plaques linearly distributed on the abdomen, following the Blaschko’s lines (Figure 1). The papules were mildly pruritic and had developed over the last 6 years. He reported that, in the last years, he had consulted several doctors and had been treated repeatedly for recurrent herpes zoster with acyclovir, with no improvement.
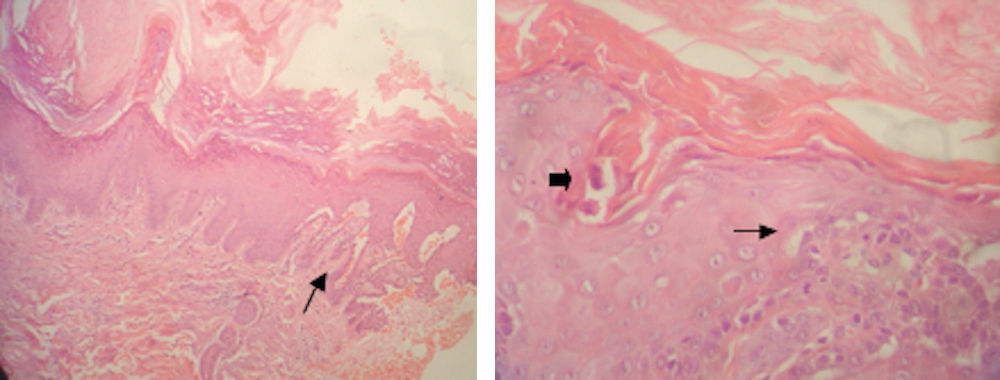
Biopsy of the plaque revealed hyperkeratosis, hypergranulosis, acanthosis, and suprabasal acantholysis associated with corps ronds, besides inflammatory infiltrate in the papillary layer of the dermis (Figure 2). Linear Darier’s disease was then diagnosed.
Histopathological study.
A - Hyperkeratosis, hypergranulosis, and irregular acanthosis with suprabasal acantholysis (arrow) (Hematoxylin & eosin, original magnification x100).
B - Grains in the stratum corneum (thick arrow) and acantholysis (thin arrow) (Hematoxylin & eosin, original magnification x400)
The patient was treated with topical clobetasol 0.05% and acitretin 25mg/per day for 2 months, with good response (Figure 3).
DiscussionLinear or zosteriform Darier’s disease was first described in 1906 and is still a rare disorder, with few cases reported in the literature. It presents as reddish-brown, pruritic, keratotic papules distributed linearly along the Blaschko’s lines.
The disease has been associated with abnormalities in the ATP2A2 gene, identified as an underlying cause, since the lead to insufficient function of the calcium-ATPase pump in the endoplasmic/sarcoplasmic reticulum, consequently causing premature keratinization and acantholysis, due to impact on the adhesion between the keratinocytes.1–3 Some authors report that UV light can be an exacerbating factor.4
Linear Darier’s disease tends to appear during the third or fourth decade of life, with no gender predilection. The most frequently affected area is the trunk. The surrounging skin is absolutely normal; some authors believe that this results from postzygotic mutation and heterozygosity for the disease, with the development of point mutations. It is also believed that in the presence of gonadal mosaicism, the mutation can be transmitted to the patient’s offspring, but it is extremely rare in the linear form.5 Differential diagnosis includes Grover’s disease, epidermal dyskeratotic nevus, and lichen striatus.
Histological examination is indispensable to confirm the diagnosis, and the disorder is indistinguishable from typical Darier’s disease in the seborrheic area: hyperkeratosis, papillomatosis, acanthosis, besides dyskeratotic keratinocytes leading to acantholysis, corps ronds, and corp grains.6 According to the literature, tretinoin, salicylic acid, and corticosteroids can be used as topical treatments. Oral therapy can include retinoids such as acitretin. Pulsed dye laser and topical adapalene have also been reported as possible alternatives. Our patient responded well to topical corticoid and oral acitretin and is still in follow-up at our department.7–9
Financial support: None.
Conflict of interest: None.