We report a case of squamous cell carcinoma originated from a sacrococcygeal tailgut cyst in a 73-year-old female patient. Tailgut cysts are generally multilocal and have a layer of either columnar, squamous or transitional epithelium, or a combination of these. This case was treated with surgical excision and radiotherapy. Cancer presentation of a congenital abnormality in old age is a rare entity. This report is the first case of squamous cell carcinoma developing in a tailgut cyst without any synchronization, as an isolated (pure) pathology.
Tailgut cysts or retrorectal cystic hamartomas are congenital lesions developed from tailgut embryonic remnants.1–3 For the differential diagnosis, epidermoid cysts, dermoid cysts, rectal duplication cysts (enteric cysts) and cystic teratomas should be considered.1–6 The underlying epithelium of epidermoid cysts are stratified squamous epithelium, and dermoid cysts are identified when a skin remnant is present on the cyst wall. Rectal duplication cysts are shielded by intestinal mucosa, and their wall contains an organized muscularis propria.2,4,7 Tail cysts, however, are multilocular, and the underlying epithelium is squamous, transitional, or a combination of both.2,4 A case of seromucous gland structures on the cyst has also been reported.8
Case ReportOur patient had a nodular mass in her sacrococcygeal skin region that had been present since her teens. She had had no complaint until recent months, when she experienced pain and growth of the mass. Physical examination revealead five pits on the surface of the swollen mass, which was fixed to the sacrum. Rectal examination revealed that the tumoral mass leaned on the posterior wall of the rectum. Magnetic resonance imaging identified a sacrococcygeal cystic tumoral mass, measuring 70mm in length and 80mm in width, near the posterior wall of the rectum and extending into the subcutaneous tissue. After tru-cut biopsy, the pathology was reported as squamous cell carcinoma. Under general anesthesia on the prone position, the tumor and all surrounding connective tissues were dissected by fusiform excision. However, the cystic portion—comprising a 30-cc mass inside the pelvic cavity, left of the rectum—could not be dissected because it was fixed to surrounding tissues (Figures 1, 2 and 3).
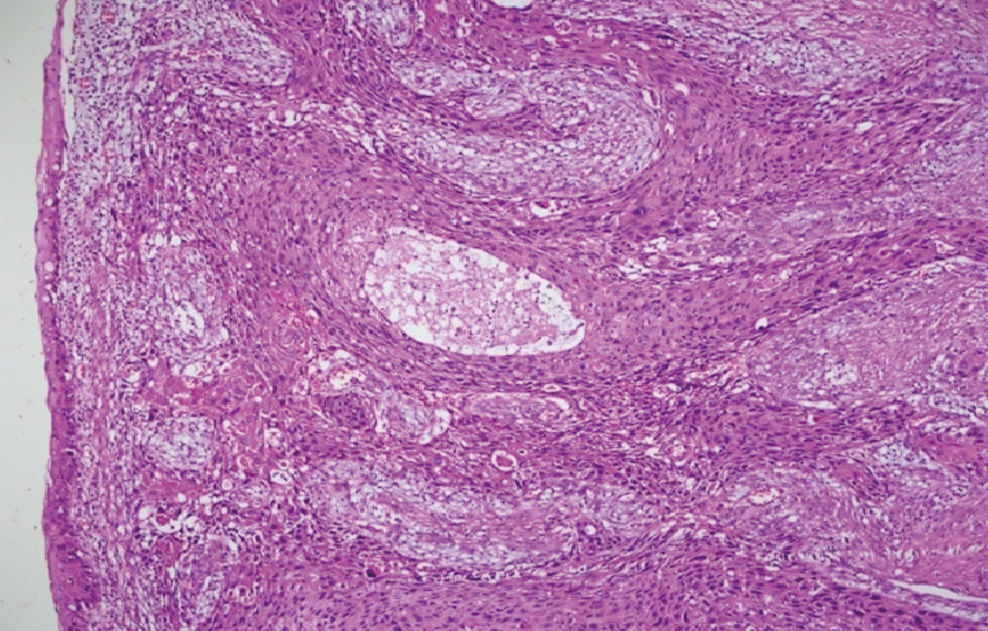
The pathology report described a tumoral mass lined by squamous eptithelium with intensive dysplasia, and a contained microscopic tumoral invasion in one site. The tumor consisted of atypical and normal squamous cells and showed keratinization in solid masses and cordons. The tumor invaded subcutaneous adipose tissue and skeletal muscle tissue. The surgical skin excision margins were reported as being clear of tumor, and the squamous cell carcinoma developed from the epithelial lining of the tailgut cyst. The large cyst was multilocular, as well as its related small cysts in the pelvic cavity, and the underlying epithelium was moderately differentiated squamous carcinoma. Intensive dysplasia and invasion were observed in many areas.
Radiotherapy was applied to the operative and residual sites of the tumor 3 months after the operation, at 6600 cGy in 30 fractions (July 05, 2015–August 17, 2015) by means of intensity-modulated radiotherapy technique. The residual mass could no longer be detected at the nine-month follow-up by PET/CT scan, but 18F-FDG uptake revealed a 15-mm nodule posterior to the right sciatic nerve near the trochanter major.
DiscussionAlthough tailgut cysts are seen in all age groups, they are most common in middle-aged women.1,2,4,7,9 They are generally asymptomatic and are diagnosed through localization in later ages. A localized lesion at low sites may be misdiagnosed as pilonidal sinus, especially when pitted lesions are present on the surface, as in our case. Symptoms associated with an enlarging mass include pain, rectal fullness, constipation, dysuria, obstructive and gynecological symptoms, as well as chronic abscess and fistula.2,4
Our 73-year-old patient had had the mass since her teens, but had recently suffered pain, possibly related to the cyst. There were no signs of either infection or discharge.
Malignant transformations in tailgut cysts, though very rare, are generally transitional cell carcinoma, carcinoid tumor and adenocarcinoma; 33 cases have been reported in the literature.1,2,3,5,7,8,10 Squamous cell carcinoma was reported previously in only one case of synchronized rectal adenocarcinoma, making ours the second case report in the literature.4 Moreover, ours is the first case report of squamous cell carcinoma developing in a tailgut cyst without synchronization, as an isolated (pure) pathology.
In the diagnosis of tailgut cysts, CT and MRI tests are helpful. The tru-cut biopsy is valuable, though it risks tumor spread and infection and could miss the localization.7 In our case, we preferred tru-cut biopsy.
The treatment of tailgut cysts is the dissection of the mass with clear surgical margins. A surgical approach is supported for the anatomical site. A posterior approach is appropriate for tumors located lower than the forth sacral vertebral level, while a transabdominal approach is appropriate for higher levels; both approaches are suitable for malignant lesions. A transvaginal approach would be used for small lesions in female patients.1,4,7
In our case, the big tumor in the presacral region was excised by posterior approach, but the cystic component near the rectum wall inside the pelvis could not be excised. Due to the patient’s advanced age, radiotherapy was chosen instead of an abdominal approach, which is associated with greater morbidity.
Financial support: None.
Conflict of interest: None.