Linear immunoglobulin A bullous dermatosis is a rare autoimmune disease that usually has an excellent prognosis in childhood; however, its control is more difficult in adults. It presents heterogeneous clinical manifestations and is frequently confused with other bullous diseases such as bullous pemphigoid and Duhring’s dermatitis herpetiformis. Dermatologists’ awareness of this disease contributes to early diagnosis and appropriate treatment. We thus report three cases of linear immunoglobulin A dermatosis in adults.
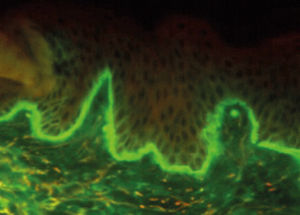
Described for the first time in the 1970s as a different entity from dermatitis herpetiformis, linear IgA dermatosis is a rare autoimmune bullous disease characterized by subepidermal blisters and linear deposition of IgA in the basement membrane zone, shown on direct immunofluorescence (DIF).1,2 Two clinical forms are known: in childhood, with a peak incidence at four to five years of age, with excellent prognosis and rarely persisting beyond puberty, and in adulthood, which occurs after puberty or after 60 to 65 years of age and presents less frequent remission.3
Considering the rarity of this disease in adults and the importance of the dermatologist’s awareness of it for early diagnosis, we report three cases of linear IgA dermatosis in adults.
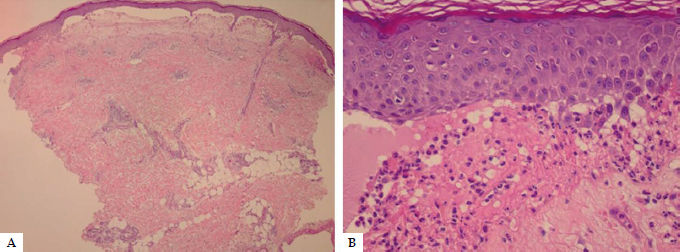
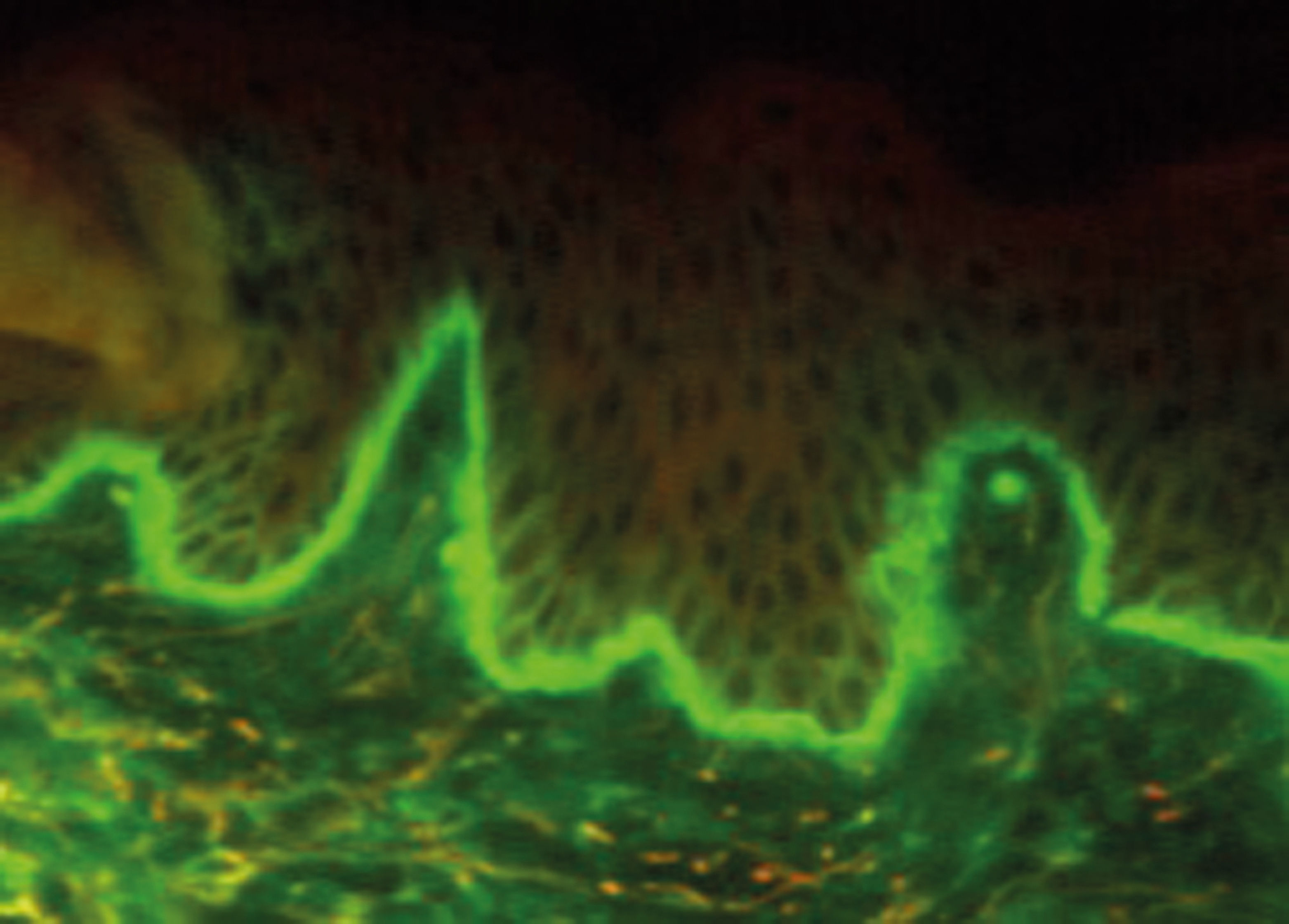
Case ReportsCase 1Female patient, 44 years, complained of lesions on her skin in the previous 50 days. On examination, she presented vesicles, blisters, and hemorrhagic crusts with an arciform configuration on her neck, trunk, and lower limbs, with no mucosal lesions (Figure 1). She reported no comorbidities or recent use of medications. Anatomopathology (AP) showed subepidermal bullous dermatosis with microabscesses in the papillary dermis, and DIF showed moderate linear IgA fluorescence in the basement membrane zone — findings consistent with linear IgA dermatosis (Figures 2 and 3). Patient was treated with prednisone (maximum dose 60mg/day, the equivalent of 1mg/kg/day) and dapsone (maximum dose 100mg/day, reduced to 50mg/day due to hemolysis). Five years after onset of the condition, she presented glaucoma, arterial hypertension, osteoporosis, and Cushingoid facies as side effects of prolonged corticosteroid therapy, and new lesions appeared with each attempt to reduce the dose. Azathioprine (100mg/day) and erythromycin (2g/day) were associated with the treatment, but both produced little response. The patient currently presents partial control of the disease, in use of prednisone (10mg/day) and dapsone (50mg/day).
Male patient, 51 years of age, reported pruritic skin lesions in the previous month. Upon examination, he presented tense blisters throughout the tegument, some with a rosette configuration (Figure 4). He reported no comorbidities or use of medications. With bullous pemphigoid and epidermolysis bullosa acquisita as the diagnostic hypotheses, biopsies were performed for anatomopathology and DIF, and patient was started on prednisone [60mg/day (0.6mg/kg)]. One month later the patient showed significant improvement in the lesions. Biopsies revealed subepidermal bullous dermatosis with the presence of linear IgA fluorescence in the basement membrane zone — findings consistent with linear IgA dermatosis. Prednisone was reduced, and dapsone was added (100mg/day). Three weeks later, the patient returned with mild hemolysis, and dapsone was reduced to 50mg/day. Tapering of prednisone and dapsone was maintained. Two and a half years after onset of symptoms, patient had achieved complete control, and the medications were suspended.
Case 3Female patient, 30 years of age, presented vesicles and blisters in the lumbar region, beginning one week previously. She was already on prednisone (40mg/day), prescribed at another service, and brought her pathology results, consistent with bullous pemphigoid. As personal history, she reported polycystic ovaries and frequent use of analgesics for headache. Her condition worsened during tapering of prednisone, with erythematous lesions covered with pruritic vesicles and blisters located on the trunk and upper limbs, some with blisters on the periphery, giving a rosette appearance and suggesting linear IgA bullous dermatosis (Figure 5). Biopsies were performed for pathology and DIF, the results of which were, respectively, subepidermal bullous dermatosis with neutrophilic content and moderate linear IgA fluorescence in the basement membrane zone, confirming this diagnosis. Prednisone (20mg/day) was prescribed. Three weeks later, dapsone (100mg/day) was started, suspended two weeks later due to lack of response, besides symptomatic hemolysis. Patient’s condition evolved with improvement after one month of prednisone, which the patient interrupted on her own. She returned one month later with relapse of the disease, and prednisone (20mg/day) was prescribed again with monthly dose tapering until suspension.
DiscussionLinear IgA bullous dermatosis is a rare autoimmune bullous disease with heterogeneous skin manifestations. There may be erythematous papules, urticaria-like plaques, or vesicobullous lesions. The latter may display an annular or arciform configuration or rosette appearance when new bullous lesions develop on the periphery of previous lesions. The disease can affect the flexor surfaces of the limbs and the trunk, as in bullous pemphigoid, or the extensor aspects of the limbs, as in dermatitis herpetiformis; in addition, oral involvement occurs in the majority of cases.4 It may be spontaneous or drug-induced, with vancomycin reported most frequently. However, there have also been reports of its emergence after the use of amiodarone, nonsteroidal anti-inflammatory drugs, acetaminophen, and antibiotics other than vancomycin, such as ceftriaxone and penicillin.5
Diagnosis is based on three criteria: i) vesicles or blisters on the skin or mucosae; ii) subepiderrmal blisters with neutrophilic infiltrate on anatomopathology; and iii) IgA deposits on the basement membrane zone with a linear pattern and absence of other immunoglobulins on DIF.2
Dapsone is the drug of choice, as in dermatitis herpetiformis. Its side effects are hemolytic anemia, leucopenia, methemoglobinemia, and altered liver enzymes. Monotherapy with dapsone is sufficient in many cases, but the association with corticosteroids and immunosuppressants such as azathioprine and cyclophosphamide may be necessary, especially due to dapsone’s side effects, which limit its daily dose, as occurred in the three cases reported here.6,7
Some cases of therapeutic success have been reported with the association of tetracycline and nicotinamide or with macrolides, such as erythromycin, as occurs with bullous pemphigoid.8,9
It is difficult to precisely define the duration of treatment, since most cases relapse during tapering of the medication, requiring a new increase. Mean treatment time of 4.6 years has been reported in cases of spontaneous linear IgA dermatosis.10
In conclusion, linear IgA dermatosis is a rare autoimmune bullous disease, frequently confused with other bullous diseases like bullous pemphigoid and Duhring’s dermatitis herpetiformis, due to the clinical heterogeneity. Correct early diagnosis is essential to provide adequate treatment.
Financial support: None.
Conflict of interest: None.