We present a case of a penile lesion with a clinical appearance similar to Mondor penile disease (thrombosis of the dorsal vein of the penis) or penile sclerosing lymphangitis. Laboratory evaluation, however, showed a solid lesion, with no vascular component to Doppler ultrasonography and no treponema to immunohistochemistry. Histological and serological tests were compatible with secondary syphilis. The authors reinforce the need for the inclusion of syphilis in the differential diagnosis of penile cord injuries.
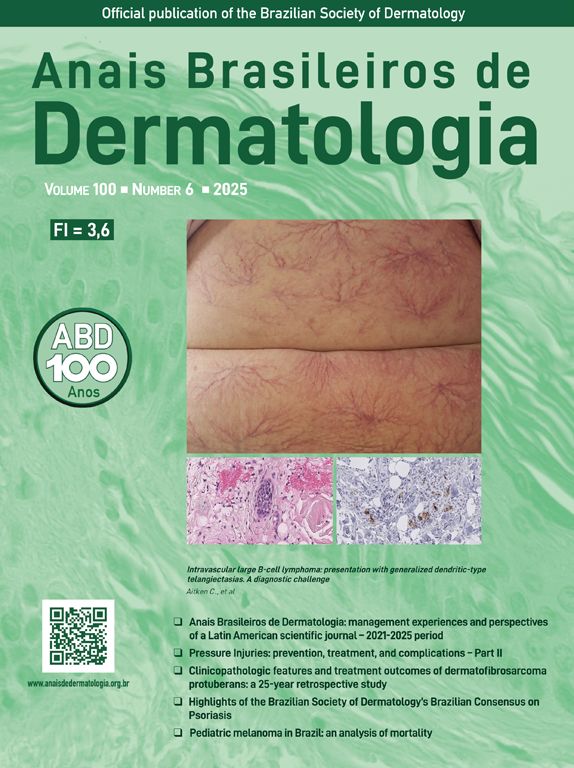
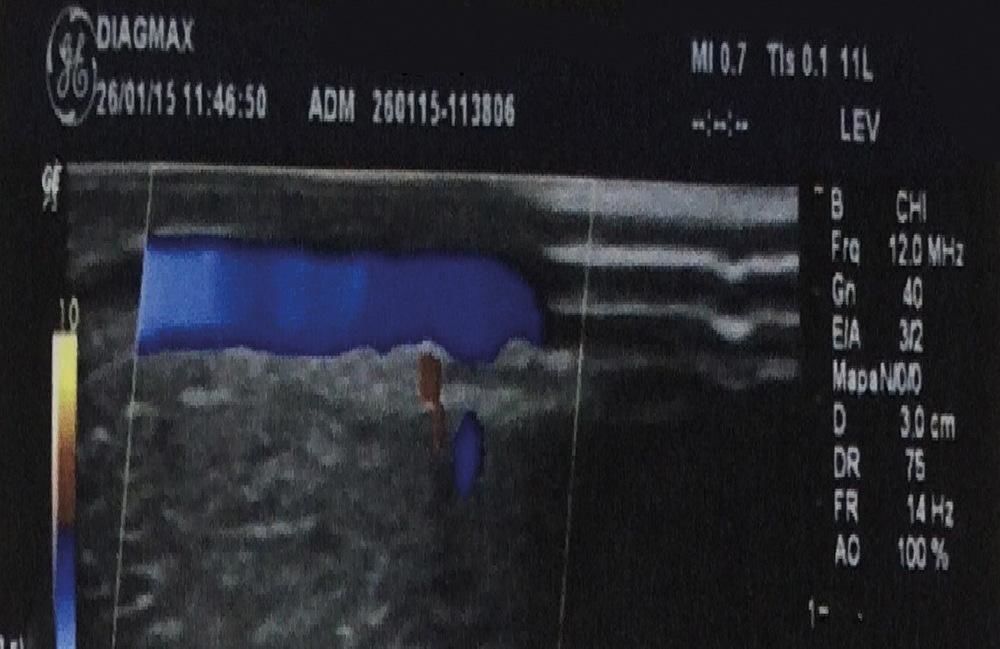
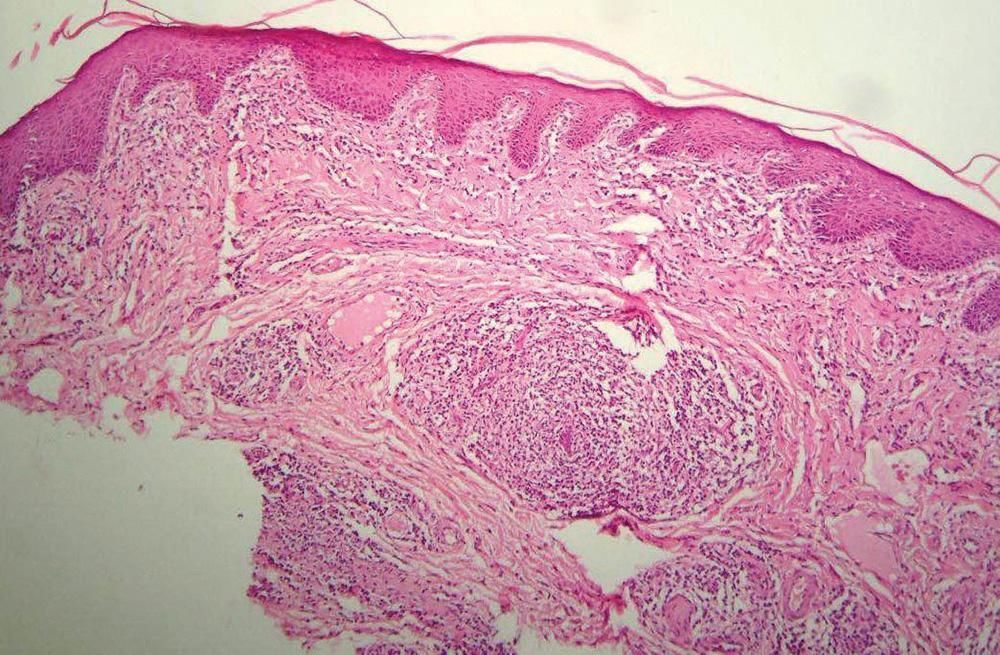
A 37-year-old patient with a painless genital lesion for 60 days. Long-term partner for many years, he reported casual unprotected sexual intercourse about four months ago. On dermatological examination, elongated, raised, shiny lesion with a cartilaginous consistency, partially surrounding sulcus was observed (Figure 1). Also detected a bilateral, firm and mobile inguinal lymphadenopathy. Serological investigation showed positive FTA-Abs and VDRL 1:32. Doppler revealed absence of thrombosis of the dorsal vein of the penis (Figure 2) or of the corpora cavernosa, describing the lesion as solid and avascular. On the histology stained by Hematoxylin & eosin (HE10x), hyperkeratosis and irregular acanthosis of the epidermis can be seen, along with edematous superficial and deep vessels, surrounded by a dense inflammatory reaction of lymphocytes, plasma cells and epithelioid cells (Figure 3).
Among the main differential diagnosis of a cord-like lesion on the penis, we highlight penile Mondor’s disease (MD) and penile sclerosing lymphangitis (PSL). MD was described in 1939 and is characterized by a superficial thrombosis of the thoracoepigastric region. In 1955, it was seen on the penis and called thrombosis of the dorsal vein of the penis.1 Penile MD is relatively rare, has a low morbidity and spontaneous resolution. It affects teenagers or young adults and the diagnosis is clinical.2 It presents as a cord-like lesion that can extend over the dorsum of the penis and be accompanied by pain.3 Doppler is useful, especially in atypical cases that involve other superficial veins, such as the circumflex vein of the penis.4 According to the histology, MD can present with 4 phases: thrombus formation, thrombus organization, recanalization and thick-walled fibrosis. It is mainly associated to traumas, sexual intercourse or vigorous physical exercises, use of vacuum devices or rings for the compression of the base of the penis.5 Another disease that has similar manifestations is penile sclerosing lymphangitis (PSL), that occurs in sexually active males between 20 and 40 years of age, with subtle onset after vigorous sexual intercourse.6 In one case, the histopathology revealed thrombosis of a lymphatic vessel, being the lymph stasis responsible for the clinical picture.7 There is no consensus regarding the differentiation between MD and PSL. Some authors suggest that they are the same condition.8 The case reported has a similar clinical picture to both, however, Doppler examination and the histology are different – there was no involvement of small veins, small arteries or lymphatic vessels. The histology was suggestive of secondary syphilis, secondary syphilis. A positive treponemal test (FTA-Abs) and VDRL 1:32 confirmed the diagnosis of early syphilis. The patient was treated with penicillin benzathine - 2, 400,000 UI and a complete cure was obseved.
Financial support: None.
Conflict of interest: None.