Atrophoderma of Pasini and Pierini is a skin disorder affecting dermal collagen and is clinically characterized by well-defined plaques of depressed skin. Histopathological changes are subtle, and in most cases, the diagnosis requires a comparative study with healthy skin from the same anatomical site. High frequency ultrasound is a useful imaging method for diagnosis of atrophic skin changes. A case is presented in which ultrasound can support the clinical and the histopathological diagnosis of atrophoderma of Pasini and Pierini.
Atrophoderma of Pasini and Pierini (APP) is a disease of unknown etiology that predominantly affects young women and is characterized by asymptomatic skin atrophy. APP manifests as a single or multiple sharply demarcated, usually hyperpigmented lesions of varying size, preferably located on the back.1 It is a matter of debate whether APP is a forme fruste or early form of morphea or an isolated entity. Some authors have suggested a role of Borrelia burgdorferi in the genesis of the disease.2 Histopathological changes are subtle, and in most cases, the diagnosis requires a comparative study with healthy skin from the same anatomical site. The epidermis appears normal, and there may be increased pigmentation of the basal layer. Recent research using multiphoton microscopy revealed alterations not in the density of either collagen or elastic fiber but in their organization.3 Skin appendages and subcutaneous tissue remain unchanged.1
Diagnostic imaging methods that allow noninvasive real-time investigation without the use of radiation are increasingly being used in dermatology. The development of high-resolution ultrasound equipment combined with high-frequency transducers has enabled the use of this technique in the diagnosis, monitoring and treatment of physiological and pathological changes of the skin and its appendages.4 Ultrasound imaging at 20 to 25 MHz allows differentiation between skin layers, and when it is combined with color or power Doppler ultrasound, it is possible to estimate blood flow in the area of interest.5
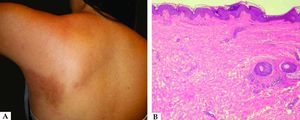
Case ReportA 30-year-old woman presented with an asymptomatic lesion on the trunk, which had persisted for three months. Physical examination revealed a single, ovoid, hyperpigmented and slightly depressed lesion, measuring 10 cm on the major axis and 5 cm on the minor axis, localized in the left infrascapular region. There were no signs of inflammation in the affected area (Figure 1A). On palpation, no induration was noted.
Laboratory tests including an examination for rheumatic activity and serology for Borrelia burgdorferi were negative.
Histopathology of lesional skin biopsy specimens revealed hyperpigmentation of the basal layer of the epidermis, mild peri-vascular inflammatory infiltrate, and collagen bundles that appear slightly hyalinized in the dermis (Figure 1B).
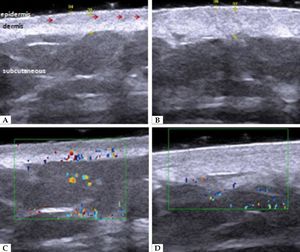
Ultrasound examination was performed using a 22-MHz linear-array transducer and Doppler color-flow imaging at 12.5 MHz (MyLab Touch; Esaote, Genoa, Italy), with application of a copious amount of aqueous gel and minimal transducer pressure. The comparative study between the left (affected) and right (healthy) scapular regions showed decreased dermal thickness in the lesion compared with normal skin (Figures 2A and B). The color Doppler imaging showed increased vascularity of the affected area (Figures 2C and D). Hypoechoic images were visible inside the dermis at both sites, indicating the presence of skin appendages.
A and B: HFUS, cross-sectional view. A: left scapular region, affected area. B: right scapular region, control. The comparative study shows decreased dermal thickness in the affected area and presence of hypoechoic regions in the dermis, suggesting the preserved skin appendages (→). Unchanged epidermis and subcutaneous tissue. C and D: Color Doppler ultrasound. C: Increased blood flow in the dermis of the affected area D: compared with the contralateral healthy area
The diagnosis of APP was made based on the correlation between clinical and ultrasound findings, because without comparative specimens, the histopathology of lesion specimens was inconclusive.
DiscussionIn high-frequency ultrasound (HFUS), morphea can be differentiated from APP by the presence, in the early stage of disease, of low echogenicity and increased skin thickness, representing edema; and in the late stage, there is decreased skin thickness and increased echogenicity, corresponding to fibrosis and skin thinning.6,7
The literature is unclear whether APP is a distinct entity or a form of localized scleroderma. Considering the findings presented in this case together with the results of Vieira-Damiani et al.,3 the authors reiterate the proposal that APP could be classified into classic and morphea-like variants.
HFUS is a useful tool for early diagnosis of atrophic skin changes, especially at early stages, in which histopathological changes are subtle and require comparative study with healthy tissue for a better definition. Thus, HFUS can support the clinical and the histopathological diagnosis, obviating the need for large biopsies or collection of a second sample.8,9 This reduces patient discomfort and the number of underdiagnosed cases, in which early initiation of treatment is important for the therapeutic response. HFUS is a noninvasive, painless procedure, and serial measurements can be used to monitor lesion progression.10 However, because its application is relatively recent in dermatology, further studies based on a higher number of patients are necessary to confirm these findings and standardize the terminology and criteria for evaluating disease progression, which would increase its applicability in routine dermatological practice.□