Secondary syphilis can have different clinical presentations, with corymbiform rash as its rarest manifestation. The disease is characterized by a central papule surrounded by smaller ones. We report the case of a man who has sex with man with corymbiform syphilis. The patient was subsequently diagnosed with HIV infection, hepatitis B, non-gonococcal urethritis, as well as infection of the central nervous system by treponema. This case not only illustrates a rare presentation of secondary syphilis, but also demonstrates the importance of further investigation of sexually transmitted infections, particularly among at-risk patients.
Syphilis is a sexually transmitted infection (STI) caused by the bacterium Treponema pallidum. The disease is divided into stages according to its duration: primary, secondary, latent, and tertiary syphilis.1 The dermatological manifestations of the secondary stage are diverse, with reports of macular, papular, nodular, and lichenoid lesions, among others. The presentation of secondary syphilis with corymbiform lesions is extremely rare. It is characterized by larger papules surrounded by smaller satellite lesions, making differential diagnosis with sarcoidosis, amyloidosis, and Sweet’s syndrome.2-4
Patients diagnosed with syphilis should be investigated for other STIs, such as HIV infection and hepatitis B and C. Studies have shown that HIV infection may be present in more than a quarter of those diagnosed with syphilis. In some regions of the United States, this figure may reach as high as 70%.5 Patients coinfected with HIV and Treponema pallidum may present with rare clinical manifestations, as well as atypical evolutions of the natural history of syphilis, such as concomitance of stages.1,6
Sexual risk behaviors and poor adherence to preventive methods make men who have sex with men (MSM) a population that is especially vulnerable to STIs.5,7 Despite global efforts over the years to contain syphilis and HIV – especially among those with risk behavior –, the occurrence of new infections among MSM continues to grow.7
We report the case of a patient with corymbiform syphilis who was also diagnosed with three other STIs during follow-up: hepatitis B, HIV infection, and non-gonococcal urethritis, as well as neurosyphilis.
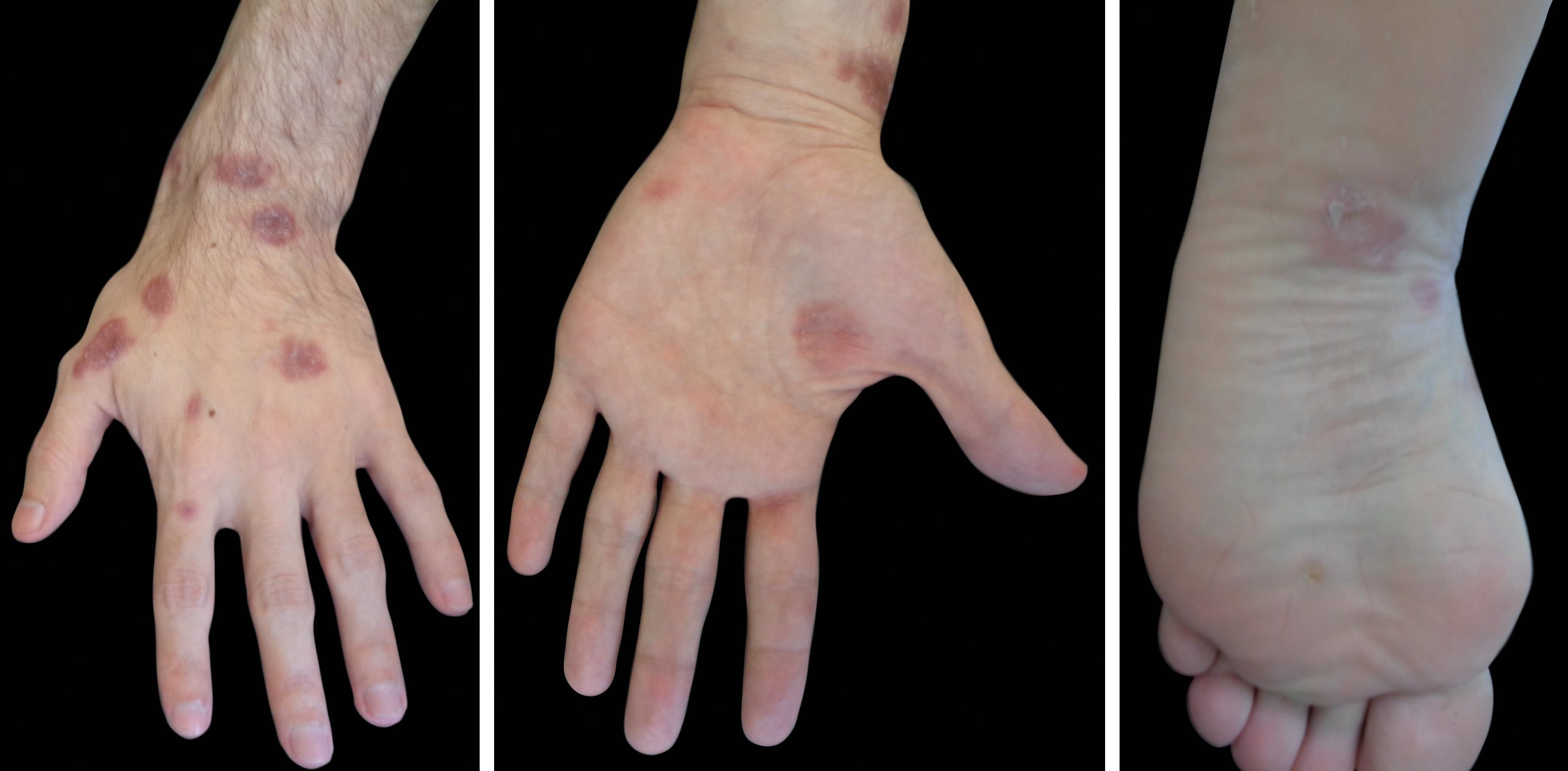
Case ReportWe report a 29-year-old MSM patient with no pathological history. He reported sudden onset of asymptomatic disseminated dermatosis characterized by erythematous papules clustered in a flowerlike arrangement (corymbiform arrangement) associated with erythematous macules, some with a squamous ring (Biett’s collarette), and annular plaques on the back of the hands. The patient reported that the lesions started on the upper limbs with posterior dissemination to the genitalia, palms, and soles after one month of evolution (Figures 1 and 2). We observed an asymptomatic ulcer with slightly raised borders and a clean base in the perianal region (Figure 3).
We considered the diagnostic hypothesis of corymbiform secondary syphilis concomitant with rectal chancre. After a biopsy of the lesion on the back of the hands, we requested serologies for HIV, hepatitis B, hepatitis C, and syphilis. The results showed VDRL positive with a titer of 1:1024, positive treponemal screening test (CMIA), positive HIV serologic test, positive Anti-HBs and Anti-HBc, and non-reactive HBsAg. Histopathological examination of the hand lesion was compatible with the clinical hypothesis of syphilis.
After prescribing a treatment with benzathine penicillin, we referred the patient to an HIV reference center due to his positive HIV and hepatitis B test results. We also requested a cerebrospinal fluid (CSF) analysis to assess syphilitic involvement of the central nervous system.
In the return visit, skin lesions evolved with progressive regression, and the anal ulcer lesion was fully healed. The patient complained of urethral discharge, dysuria, and increased testicular volume four days before the consultation. On examination, in addition to the clear egg-white color urethral discharge, we observed scrotal swelling and pain on palpation of the right testicle and epididymis (Figure 4). Bacterioscopic analysis of the urethral secretion smear showed inflammatory cells lacking gram-negative diplococci. CSF analysis showed a clear and colorless sample with 16 cells/mm3 (84% lymphocytes, 1% eosinophils, 6% monocytes, 1% neutrophils, 8% plasma cells), protein level of 63mg/dl, glucose 53mg/dl, positive Pandy’s test, and VDRL positive with a titer of 1/2. These findings allowed the confirmation of infection of the central nervous system by treponema.
We introduced treatment of urethral discharge and epididymitis with ciprofloxacin 500mg every 12 hours for 14 days associated with azithromycin 1g in a single dose. We explained the diagnosis of neurosyphilis to the patient and talked about the need for hospitalization to receive intravenous crystalline penicillin. We scheduled return in one week for hospitalization, but the patient failed to attend the consultations despite our active search.
DiscussionCurrently, we are facing a global epidemic of syphilis.1 With this increase in cases, dermatologists have been confronted with atypical clinical manifestations, such as the case of corymbiform syphilis. A literature search on corymbiform syphilis yields only three results in the last 40 years, showing the rarity of this clinical presentation, which is demonstrated by the present case.3 The word corymbiform derives from the Greek “korymbos”, said of lesions grouped around a single, usually larger, lesion.4
Although it is a rare clinical presentation, corymbiform syphilis behaves like other forms of secondary disease, with lesions spread throughout the body and may be associated with lymphadenomegaly and fever.2
The Brazilian Ministry of Health (MS) instructs physicians to offer HIV, hepatitis B and C, and syphilis examinations when diagnosing STIs.3 The present case clearly illustrates the importance of such investigations.
Most syphilis outbreaks occur in urban MSM communities. There are a number of recognized risk factors for syphilis infection among MSM, which include the occurrence of multiple anonymous sexual partners, increased popularity of the Internet as a sexual partner search tool, and use of alcohol and other recreational drugs before or during sex.5,7 In parallel to these facts, UNAIDS estimates indicate that while 0.39% of the general population is living with HIV in Brazil, the prevalence among MSM grows to 10.5%.8 According to the MS, there has been a trend towards an increase in the proportion of MSM cases in the last ten years, from 35.3% in 2006 to 45.4% in 2015.9
HIV-infected patients who contract syphilis may present with atypical clinical manifestations. Over 70% of patients have more than one hard chancre in the primary stage of syphilis, and 25% have concomitant hard chancre with secondary lesions, as in the present case.6
Approximately one third of patients with early syphilis have Treponema pallidum invasion into CSF regardless of their HIV serology. However, most new cases of neurosyphilis in HIV-infected individuals are identified in the early stages of syphilis, as in our patient. In addition, a recent correlation has been reported between abnormal CSF findings suggestive of neurosyphilis and advanced HIV disease.6
In Brazil, STI clinical management is based mainly on the syndromic approach, since the molecular diagnosis of STI is not routinely available in the Brazilian public health system.3,10 The genital discharge presented by our patient was clinically characterized as non-gonococcal, which was confirmed by the absence of gram-negative diplococci in the bacterioscopic examination. In this case, the therapeutic approach indicated is treatment for chlamydia – responsible for 50% of these cases – with return scheduling for improvement evaluation.3
The present case is notable not only for the rarity of this secondary syphilis presentation, but also for demonstrating the importance of the investigation of other STIs, especially among at-risk patients. We must be prepared to investigate, diagnose, and treat complex cases such as the one described here.
Financial support: None.
Conflict of interest: None.