Isotretinoin is a retinoid that is effective in the treatment of moderate to severe acne; however, there may be resistance to its use due to fear of adverse psychiatric effects. In turn, acne has a significant psychological impact.1 In the present study, patients using oral isotretinoin for moderate to severe acne were assessed regarding the evolution of depressive symptoms and their correlations.
This was a pragmatic, prospective study including patients of both sexes and over 13 years old, recruited in the period from 2015 to 2017, with indication for treatment with oral isotretinoin for acne at the Dermatology Service of Hospital das Clínicas of Universidade Estadual Paulista. The study was approved by the ethics committee (proceeding No. 712,311).
The patients were evaluated before the start of isotretinoin and in months 1, 3, 6, 9, and 12, until the final date of use of the medication. Patients were evaluated according to demographic data; severity of acne, according to a scale based on the 2002 FDA classification and quantification of lesions on the left hemiface; severity of scars, based on the Acne Scar Scale (AScSc) published in 2007; and the Cardiff Acne Disability Index (CADI) and Beck's depression scale.2–5
The mucocutaneous adverse effects of isotretinoin, satisfaction with treatment, and treatment-related disability were assessed by questions and Likert-type scales developed by the researchers (not validated).
Depression scores were compared between different consultations in a bivariate fashion, and by generalized mixed models with a gamma distribution for better adjustment, considering the abnormality of the dependent variable. Multivariate models were defined by including variables with p<0.2 in the bivariate analyses. The normality of the distributions was assessed by the Shapiro–Wilk test, and the reliability of the scores used was verified by Cronbach's alpha. The significance level was set at p<0.05.
The study included 42 participants who had at least one consultation after starting treatment; the sample included 18 women (43%), with a median age of 18 (p25–p75: 16–21) years and acne duration of four (2–6) years. The mean Cardiff score was 7.79 (SD=3.62) and the median Beck score was 7.5 (2–16).
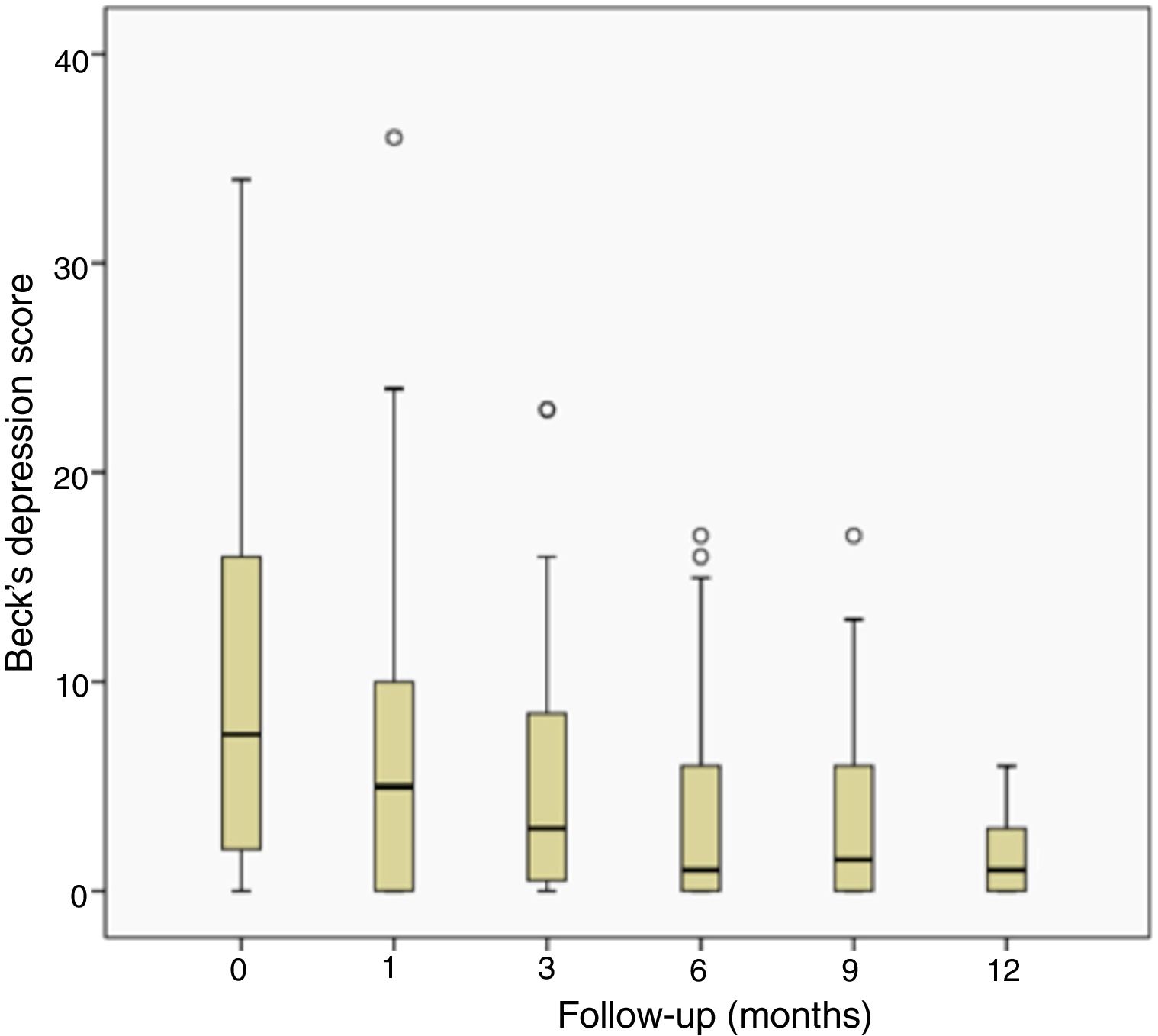
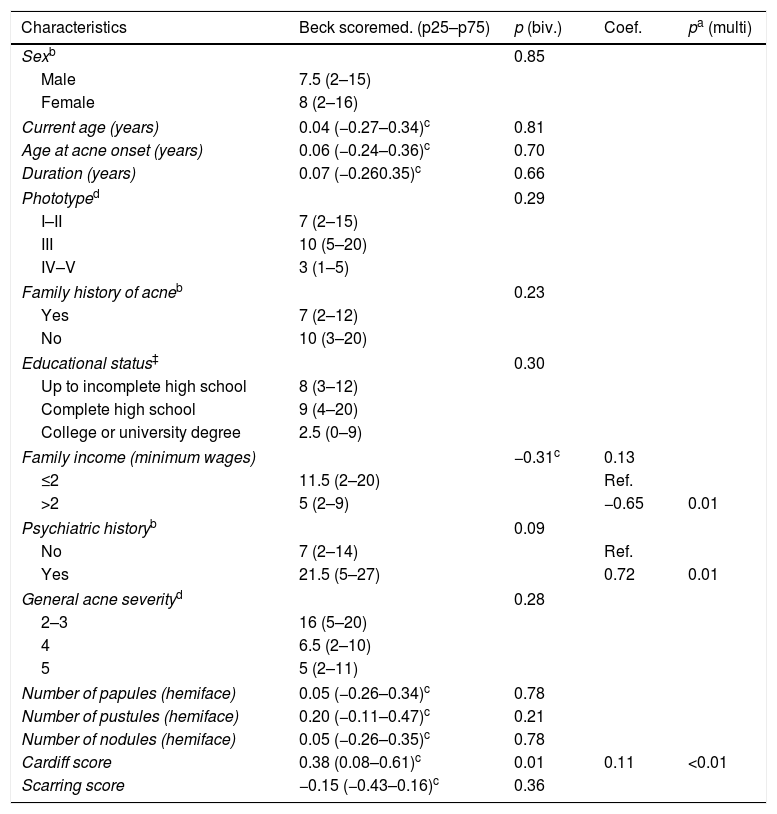
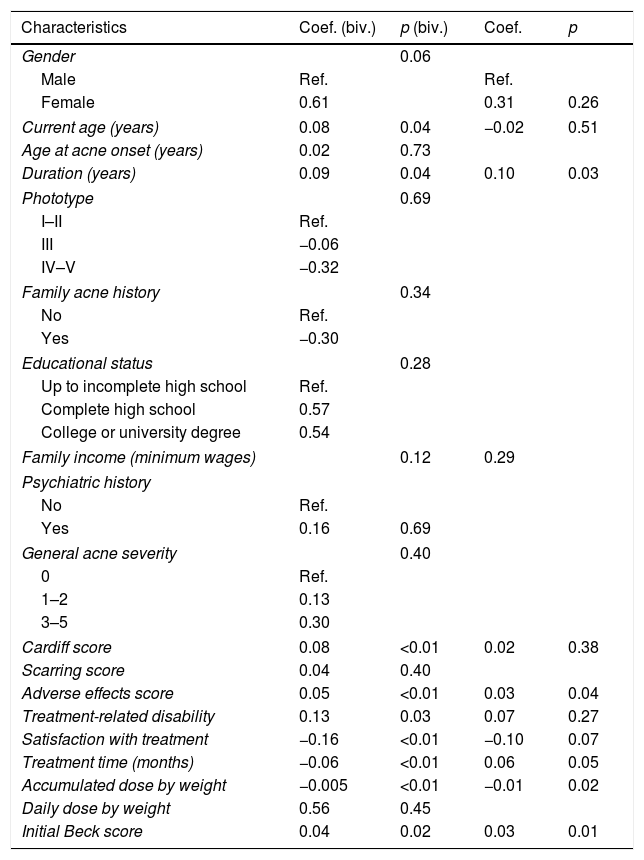
Figure 1 illustrates the regression of the Beck score during treatment. The correlation between the Beck score and CADI at the start of treatment was 0.38 (Spearman's rho; p=0.01) and between the Beck score and the clinical severity of acne, it was −0.19 (Spearman's rho; p=0.24). Table 1 demonstrates the influence of the variables studied on the Beck score at the beginning of treatment; family income, psychiatric history, and Cardiff score stand out. Table 2 presents the influence of these variables during treatment; previous duration of acne, intensity of mucocutaneous adverse effects, accumulated dose of isotretinoin, and initial Beck score stand out. All scores used in the study showed acceptable or superior reliability (Cronbach's alpha>0.7).
Association between clinical, demographic, and psychometric variables and Beck's depression score at the beginning of treatment (n=42)
| Characteristics | Beck scoremed. (p25–p75) | p (biv.) | Coef. | pa (multi) |
|---|---|---|---|---|
| Sexb | 0.85 | |||
| Male | 7.5 (2–15) | |||
| Female | 8 (2–16) | |||
| Current age (years) | 0.04 (−0.27–0.34)c | 0.81 | ||
| Age at acne onset (years) | 0.06 (−0.24–0.36)c | 0.70 | ||
| Duration (years) | 0.07 (−0.260.35)c | 0.66 | ||
| Phototyped | 0.29 | |||
| I–II | 7 (2–15) | |||
| III | 10 (5–20) | |||
| IV–V | 3 (1–5) | |||
| Family history of acneb | 0.23 | |||
| Yes | 7 (2–12) | |||
| No | 10 (3–20) | |||
| Educational status‡ | 0.30 | |||
| Up to incomplete high school | 8 (3–12) | |||
| Complete high school | 9 (4–20) | |||
| College or university degree | 2.5 (0–9) | |||
| Family income (minimum wages) | −0.31c | 0.13 | ||
| ≤2 | 11.5 (2–20) | Ref. | ||
| >2 | 5 (2–9) | −0.65 | 0.01 | |
| Psychiatric historyb | 0.09 | |||
| No | 7 (2–14) | Ref. | ||
| Yes | 21.5 (5–27) | 0.72 | 0.01 | |
| General acne severityd | 0.28 | |||
| 2–3 | 16 (5–20) | |||
| 4 | 6.5 (2–10) | |||
| 5 | 5 (2–11) | |||
| Number of papules (hemiface) | 0.05 (−0.26–0.34)c | 0.78 | ||
| Number of pustules (hemiface) | 0.20 (−0.11–0.47)c | 0.21 | ||
| Number of nodules (hemiface) | 0.05 (−0.26–0.35)c | 0.78 | ||
| Cardiff score | 0.38 (0.08–0.61)c | 0.01 | 0.11 | <0.01 |
| Scarring score | −0.15 (−0.43–0.16)c | 0.36 | ||
Association between clinical, demographic, and psychometric variables and Beck's depression score during treatment (n=107)a
| Characteristics | Coef. (biv.) | p (biv.) | Coef. | p |
|---|---|---|---|---|
| Gender | 0.06 | |||
| Male | Ref. | Ref. | ||
| Female | 0.61 | 0.31 | 0.26 | |
| Current age (years) | 0.08 | 0.04 | −0.02 | 0.51 |
| Age at acne onset (years) | 0.02 | 0.73 | ||
| Duration (years) | 0.09 | 0.04 | 0.10 | 0.03 |
| Phototype | 0.69 | |||
| I–II | Ref. | |||
| III | −0.06 | |||
| IV–V | −0.32 | |||
| Family acne history | 0.34 | |||
| No | Ref. | |||
| Yes | −0.30 | |||
| Educational status | 0.28 | |||
| Up to incomplete high school | Ref. | |||
| Complete high school | 0.57 | |||
| College or university degree | 0.54 | |||
| Family income (minimum wages) | 0.12 | 0.29 | ||
| Psychiatric history | ||||
| No | Ref. | |||
| Yes | 0.16 | 0.69 | ||
| General acne severity | 0.40 | |||
| 0 | Ref. | |||
| 1–2 | 0.13 | |||
| 3–5 | 0.30 | |||
| Cardiff score | 0.08 | <0.01 | 0.02 | 0.38 |
| Scarring score | 0.04 | 0.40 | ||
| Adverse effects score | 0.05 | <0.01 | 0.03 | 0.04 |
| Treatment-related disability | 0.13 | 0.03 | 0.07 | 0.27 |
| Satisfaction with treatment | −0.16 | <0.01 | −0.10 | 0.07 |
| Treatment time (months) | −0.06 | <0.01 | 0.06 | 0.05 |
| Accumulated dose by weight | −0.005 | <0.01 | −0.01 | 0.02 |
| Daily dose by weight | 0.56 | 0.45 | ||
| Initial Beck score | 0.04 | 0.02 | 0.03 | 0.01 |
The vast majority of patients (6/7) who presented clinically significant scores on the Beck scale (<19) presented as such at treatment initiation; an improvement in the scores of most of these patients was observed in subsequent evaluations. Interestingly, no correlation was observed between this and the clinical severity of acne at the initial moment, indicating underlying factors in the psychological impact of the disease, such as socioeconomic level.
During treatment, there was an early and significant reduction in depression scores in the first months, suggesting that the expectation on and perception of continued improvement may have an important psychological impact.
Regarding depressive symptoms during treatment, no significant association was observed with the severity or disability related to acne, but rather with greater adverse effects of treatment, longer previous duration of acne, higher initial depression scores, and lower accumulated doses of isotretinoin.
The identification of the association between the intensity of mucocutaneous adverse effects and depressive symptoms highlights the importance of being attentive to these factors, applying measures to effectively mitigate them and guiding the patient in advance, especially at the beginning of treatment.
The study has limitations regarding loss to follow-up and irregular use of medication by some participants, in addition to being monocentric. In turn, this was an observational study of a pragmatic character, and the mixed statistical models allowed the robust analysis of the series with missing data. Furthermore, the study design made it possible to evaluate internal and temporal variations in the variables studied, with results compatible with the available literature. It also provides new information on the profile of depressive symptoms in patients using oral isotretinoin for the treatment of acne.
Financial supportNone declared.
Authors’ contributionsPriscilla Pereira Luvizotto: Approval of the final version of the manuscript; conception and planning of the study; elaboration and writing of the manuscript; obtaining, analyzing,and interpreting the data; critical review of the literature; critical review of the manuscript.
Juliano Vilaverde Schmitt: Statistical analysis; approval of the final version of the manuscript; conception and planning of the study; elaboration and writing of the manuscript;obtaining, analyzing, and interpreting the data; effective participation in research orientation; critical review of the literature; critical review of the manuscript.
Conflicts of interestNone declared.
How to cite this article: Luvizotto PP, Schmitt JV. Depressive symptoms before and during treatment of acne with isotretinoin and its correlations: a prospective study. An Bras Dermatol. 2020. https://doi.org/10.1016/j.abd.2020.04.008
Study conducted at the Department of Dermatology and Radiotherapy, Faculdade de Medicina, Universidade Estadual Paulista, Botucatu, SP, Brazil.