Dear Editor,
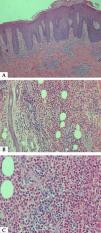
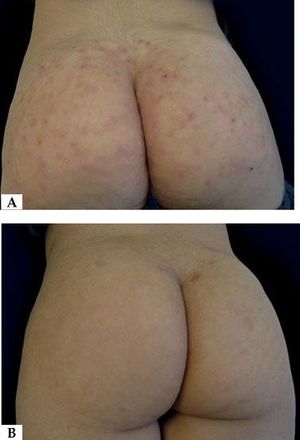
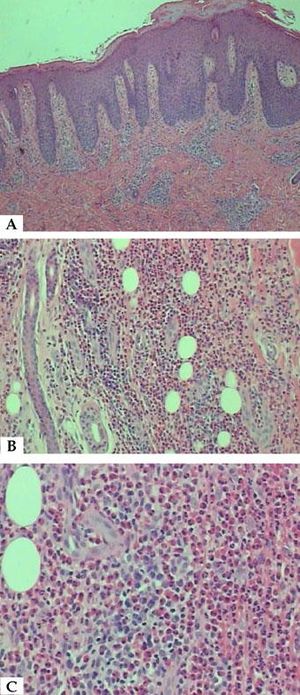
Eosinophilic panniculitis (EP) is an uncommon panniculitis and is considered as a reactive process associated with different clinical conditions.1 Among such conditions we find atopic dermatitis, contact dermatitis, arthropod bites, erythema nodosum, injection granuloma, leukocytoclastic vasculitis, lymphomas (T and B), autoimmunity and infectious processes (Gnathostoma, Streptococcus and Toxocara).1,2 We describe herein the case of a 5-year-old girl with papules and nodules in the gluteal region (Figure 1), with an evolution of 3 months, accompanied by bilateral inguinal adenopathy, whose laboratory and anatomopathological investigation indicated eosinophilic panniculitis associated with toxocariasis. In the laboratory analysis, cell blood count (CBC) showed eosinophilia of 2,813 eosinophils (20.4% of total leukocytes), serum IgE at 928 UI/mL (normal 393 UI/mL), and IgG (ELISA) reagent for Toxocara canis. Proteinogram, hepatic, renal and thyroid function tests were normal. Anti-HIV, anti-HCV, VDRL and anti-nuclear factor were non-reactive. Parasitological stool examination, direct mycological test and culture (for fungi and mycobacteria) were negative. Qualitative urine test was normal. Imaging tests (abdominal ultrasound and chest X-ray) did not show any abnormality. Skin biopsy revealed a dense inflammatory infiltrate, predominantly eosinophilic in the papillary and reticular dermis, as well as in the septa and lobules of the subcutaneous adipose tissue (Figure 2). The histophatological diagnosis was compatible with EP. After reagent serology (ELISA) for Toxocara canis, intense eosinophilia and compatible histopathology, the diagnosis of EP associated with occult toxocariasis was confirmed. The patient was treated with albendazole 10mg/kg/day for 10 days, with significant reduction of pruritus and cutaneous lesions after 30 days and complete resolution of the condition after 3 months. Control CBC after 60 days of treatment showed significant decrease in eosinophils. Follow-up continued for 6 months, with no evidence of relapse.
A - Skin showing acanthosis, parakeratosis and inflammatory infiltrate in superficial and deep dermis (Hematoxylin & eosin, x40), B - Hypodermis with dense inflammatory infiltrate, predominantly eosinophilic (Hematoxylin & eosin, x100) and C - Eosinophils in septa of subcutaneous adipose tissue (Hematoxylin & eosin, x200)
EP was first described in 1985 by Burket and Burket.2 Patients usually present subcutaneous nodules that involve the trunk, extremities or scalp, but papules, pustules and even ulcers may also be observed. Histopathological studies are necessary for diagnostic confirmation.1 The peak of EP incidence is between the third and sixth decades of life.3 EP is rare in childhood, and the series with the most cases contain no descriptions of pediatric patients.1,2 Association of eosinophilic panniculitis with toxocariasis was documented by Rook and Taijorton in 1972, in a 72-year-old patient with peripheric eosinophilia, subcutaneous nodules, pruritus and bilateral inguinal adenopathy; the nodule biopsy revealed panniculitis with eosinophilic infiltrate. The fluorescence antibody test for Toxocara was positive, and after treatment, the patient presented complete resolution of eosinophilia and cutaneous lesions.3 Cases prior to such publication are inconsistent because they had neither a biopsy nor a confirmatory test for toxocariasis. There are two other confirmed cases of EP associated with toxocariasis in adults, both simulating rheumatic diseases.4
Histopathological changes of EP consist of intense infiltration of eosinophils in lobules and septa, extending to the reticular dermis or fascia. Flame figures and small areas of subcutaneous necrosis can also be found. Vasculitis is not usually seen by routine light microscopy.2
Once the diagnosis of EP has been established, associated clinical conditions should be investigated. Cases with infectious factors are more frequently related to toxocariasis and gnathostomiasis.2 Considering the high prevalence of infestation in the Brazilian population, toxocariasis should always be considered when patients present eosinophilia and/or related symptoms. Human toxocariasis can be classified as visceral larva migrans, ocular and neurological larva migrans, asymptomatic toxocariasis and ocult toxocariasis.5 In the classic systemic subtype, patients usually present fever, anemia, leukocytosis, nausea, hepatomegaly and pulmonary symptoms in addition to abnormalities in proteinogram, eosinophilia and positive serology. The serological diagnosis is made by ELISA, which uses Toxocara excretion-secretion antigens and has high sensitivity and specificity, varying according to the antigens tested. In the case reported here, the absence of hepatomegaly, fever, proteinogram changes and pulmonary symptoms excluded the classical form of to-xocariasis. Conversely, eosinophilia, pruritus, cutaneous lesions, and lymphadenitis, as well as the ELISA test reagent for Toxocara canis and the excellent response to therapy confirmed the occult subtype of toxocariasis.5 The treatment for toxocariasis may include albendazole, ivermectin or thiabendazole. The first medication is preferable due to better distribution through tissues after metabolized.
In endemic countries for toxocariasis, such as Brazil, the clinical presentation of pruritic nodules associated with eosinophilia should suggest the possibility of EP associated with toxocariasis. □