Dear Editor,
Lichen planus pigmentosus (LPP) is a rare variant of lichen planus, characterized by chronic acquired hyperpigmented, dark brown to grey, macular pigmentation located on sun-exposed areas of the face, neck, and flexural folds. Clinically, it differs from classical lichen planus by the longer clinical course and rare involvement of the scalp, nail, or mucosal area. Linear LPP, probably related to Blaschko's lines, is an uncommon subtype of LPP, with only a few cases of facial involvement reported.
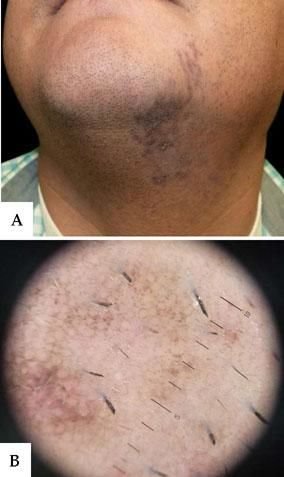
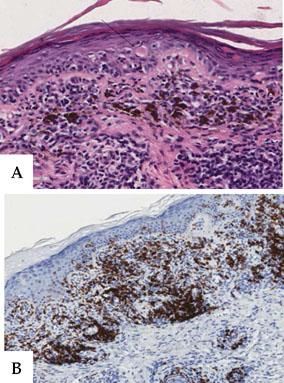
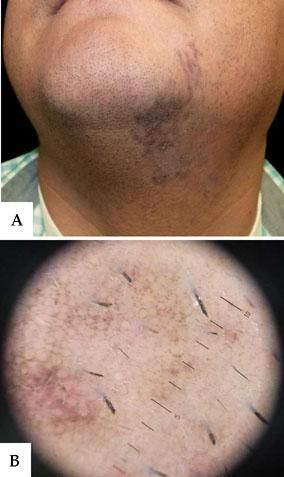
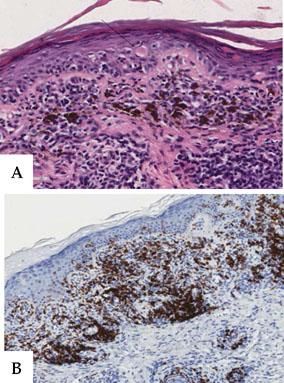
A 38-year-old male patient from El Salvador (Fitzpatrick skin type III) presented with a six-month history of slightly pruritic lesions on the chin and neck. He was not taking any medications or using cosmetics. He reported no history of excessive sun exposure or trauma on the lesion site. Physical examination revealed dark brown macules from the left side of the chin to the underside of the jaw, along the neck, with a linear distribution following Blaschko's lines (Figure 1A). We observed no other skin lesions and the oral mucosa and nails were not involved. Dermoscopy showed bluish-grey dots, globules, and exaggerated pseudoreticular network (Figure 1B). Routine laboratory data - including blood cell count, biochemistry, and serology for hepatitis B and C - were within normal ranges. Skin biopsy revealed epidermal thinning, basal cell degeneration with some apoptotic keratinocytes cells and numerous melanophaghes, pigment incontinence, and a lichenoid infiltration into the dermis (Figure 2A), predominantly composed of CD8+ T lymphocytes (Figure 2B), consistent with a diagnosis of linear LPP. The patient was treated with topical corticosteroid, with improvement of the lesions after two months.
A - Detail of vacuolar degeneration of the basal layer with apoptotic keratinocytes (black arrow) in the epidermis; dense lymphohistiocytic infiltration into the dermis with numerous melanophages and pigment incontinence (hematoxylin-eosin stain x 40). B - The infiltrate was predominantly composed of CD8+ T lymphocytes (immunohistochemical staining for CD 8 x 20)
The term LPP was coined in India by Bhutani et al. in 1974. Although LPP is frequently encountered in Indians, it also tends to occur in other racial and ethnic groups, mainly in dark-skinned Latin American, Asian, and Middle Eastern populations. The disease usually affects the middle-aged population with a female preponderance. Clinically, it is characterized by the insidious onset of bilateral, symmetrically distributed brown to gray or gray-blue macules in sun-exposed areas and flexural folds, with or without slight pruritus. Diffuse, reticular, blotchy, perifollicular and annular forms have been reported with the diffuse type being the most common. LPP has been associated with other variants of lichen planus, as well as endocrinopathies, autoimmune disease, and hepatitis C virus infection. The condition has been linked to sun exposure and topical agents such as mustard oil, amla oil, henna, hair dye, and nickel. Histopathological findings of LPP include atrophy of the epidermis with vacuolar degeneration of the basal layer and a perivascular lymphohistiocytic infiltration or lichenoid infiltrate in the papillary dermis. Dermal melanophages and pigmentary incontinence are also characteristically seen in LPP.1 The intensity of inflammation is higher in early lesions and show an inverse relation with the duration of the disease. Gray-brown or gray-blue dots and globules are the most frequent dermoscopic finding, reflecting pigment incontinence and melanophages in the dermis, followed by an exaggerated pseudoreticular pattern. Although the cause of LPP is unknown, as in lichen planus, an immune mechanism mediates its development. An autoimmune attack is generally accepted, as demonstrated by the inflammatory infiltrate of T-lymphocytes with varying populations of CD4+ and CD8+ cells. The autoreactive CD8+ T-lymphocytes are implicated as the effector cells, which cause degeneration and destruction of keratinocytes, causing intense pigmentary incontinence. In fact, the lichenoid infiltrate is predominately composed of CD8+ lymphocytes.
Linear LPP is considered a subtype of LPP. It shows a unilateral distribution, following one or several Blaschko's lines. The condition can manifest itself in a linear, segmental, or zosteriform distribution and follow a blaschkoid S-shaped pattern, or a combination of these. In a series with 33 cases of LPP in adults, 6% of them presented in a linear pattern.1 The first description of unilateral LPP presenting in a zosteriform distribution was in 1993. Since then, only 20 cases have been reported in the literature, being the segmental pattern among the most infrequent cases.2-5 Most cases occur in adults. Only one pediatric patient has been reported.4 In general, the trunk is the most frequently affected location in blaschkoid and segmental patterns, while the face and limbs are mainly affected in linear LPP. A case reported a bilateral linear pattern associated with hepatitis C virus infection.3 Only three previous cases of linear LPP on the face have been well described. The lesions affected the forehead, the nose,4 and, in one patient, the chin and neck, similar to our case.5 The linearity of the lesions in LPP is probably related to Blaschko's lines, which suggests that the predisposition to develop LPP might be determined during embryogenesis. Blaschko's lines are thought to reflect T-lymphocytic migration and the clonal expression during embryogenesis of the skin. The genetic mosaicism in an acquired Blaschko-linear inflammatory dermatosis could be responsible for the cutaneous antigenic mosaicism that may induce a mosaic T-cell response according to the trigger of viral infection or drugs.
The differential diagnosis of linear LPP includes other acquired dermatosis presenting with linear distribution, such as linear lichen planus, lichen striatus, and postinflammatory hyperpigmentation. In lichen planus, purplish papules and plaques are usually present, and, although the histopathological findings are similar, the epidermis shows a characteristic "saw tooth" pattern of epidermal hyperplasia and parakeratosis with thickening of the granular cell layer. Moreover, melanin incontinence is more prominent in LPP than in classic lichen planus. Lichen striatus usually occurs in children between 4 months and 15 years of age and is rare in adults. Patients with lichen striatus typically present with scaly erythematous papules in a linear distribution, mainly on the limbs, showing a perivascular and a periadnexal lymphocytic infiltrate on histopathology.
As in other variants of LPP, treatment of linear LPP consists of topical steroids, tacrolimus, depigmenting agents, photoprotection, and Q-switched Nd-YAG laser.
We reported the fourth case of linear LPP located on the face and neck. This condition should be considered in the differential diagnosis of a linear pigmentary disorder.
AcknowledgementsWe would like to thank Dr. Monserrat Franco-Muñoz for her help in this work.