Candidiasis is the most common opportunistic fungal infection of the oral cavity caused by fungi of the genus Candida and usually associated with immunosuppressed individuals.
Objectives:To evaluate the presence of oral candidiasis and identify the presence of Candida spp. in liver transplant recipients and assess the association between the presence of the fungus and sociodemographic variables, dietary habits and environmental exposure.
Methods:A cross-sectional study was performed with 49 patients who had undergone liver transplants at Hospital São Vicente de Paulo in Passo Fundo - RS. Patient information was collected to obtain sociodemographic data, eating habits and environmental exposure. Fungal infections were screened by oral clinical examination and the presence of Candida spp by the collection of oral samples with a sterile swab, seeded in Sabouraud Dextrose Agar, incubated at 25°C and observed at 48 hours. To identify Candida albicans, the germ tube test was performed.
Results:In 49 patient samples, 39% had the yeast of the genus Candida isolated and, of these patients, 12% had candidiasis, 66% of atrophic type and 34% pseudomembranous. Eleven yeast species were (58%) Candida non-albicans and eight (42%) Candida albicans.
Study Limitations:The present study presents as a limitation the inclusion of patients in different stages of immunosuppression.
Conclusion:The high incidence of Candida non-albicans in the oral cavity of transplant patients with a long period of transplantation is warning to a more effective control of the health of these individuals, especially those with older age.
Scientific and technological advances in medicine are prolonging the life of individuals, allowing severely ill patients to live longer, increasing the population at risk, in other words, patients with immunosuppressant conditions, making them more vulnerable to fungal infections.1-3 This population includes people with the human immunodeficiency virus (HIV), solid organ recipients or blood cell transplant and we should also take into consideration the appearance of new more potent immunosuppressants, the use of invasive therapeutic technique in intensive care units, the wide use of broad-spectrum antibiotics and the more aggressive chemotherapy for malignancies (causing mucositis and neutropenia).4,5
The incidence and severity of such infections as well as the causative pathogenic agents could be related to many risk factors of the patient such as underlying diseases, immunosuppression state and, even, the individual’s geographical location.3,6 With the introduction of more effective prophylactic strategies and the refinement in the immunosuppression regimens, the number of infectious complications after organ transplantation has been decreasing, however, infections remain as one of the life-threatening complications.6
Candidiasis is the most common fungal infection of the oral cavity, caused by fungi of the genus Candida, particularly Candida albicans, even though other species could be involved. Usually, the oral infection by Candida species is associated to immunocompromised individuals and it is characterized as an opportunistic infection.7
Oral candidiasis is among the indicators of immunodeficiency and the last decades studies in many countries have shown a change in the epidemiology of Candida spp. infections, with an increased incidence of Candida non-albicans such as C. glabrata, C. tropicalis, C. parapsilosis and C. krusei. A concerning tendency is the significant increase of strains resistance to many antifungals of the azoles and echinocandin classes. Besides, two thirds of candidemia are seen outside intensive care units.8,9 This epidemiological change has a significant impact in the therapeutic options for the initial and definitive treatment of this condition.10-12 However, the little information available regarding opportunistic infections in patients outside intensive care units are relevant to guarantee the survival of these individuals.
In view of the panorama of the problem discussed, the objective of this study is to evaluate the presence of oral candidiasis and identify the fungi of the genus candida in liver recipients, as well as analyze the association between the presence ofCandida spp. and sociodemographic, dietary habits and environmental exposure variables.
MethodsEthical aspectsThe study was preceded by the approval of the committee of ethics in research (CEP) under the number 1.216.546, following the ethical aspects of the resolution 466/12 of the Conselho Nacional de Saúde.
Design, period and place of the studyThis was a cross-sectional study performed from September to October 2015.
Population and sampleAll patients (n = 49) who underwent a liver transplant, older than 18 years of age and who consented in participating of the study were included.
Collection of epidemiological dataThe collection of data was conducted one single time under the supervision of the physician in charge. A standardized questionnaire was applied according to what was proposed by Sabadin et al.13, with data of sociodemographic variables (age, sex, state of residency, marital status, current professional activity, individual income, time from the transplant, reason for transplant); dietary habits and environmental exposure variables (lived in or traveled to areas with endemic mycosis or parasitic infections, exposure to pets, exposure to children younger than 10 years of age, water used to drink, habit of eating raw meat, non-pasteurized milk and milk products, seafood, and the presence of cutaneous abnormalities/conditions-infectious processes caused by fungi on the skin and/or nails).
Collection of data for microbiologyAn oral clinical examination was performed to evaluate the presence of oral candidiasis and of fungi of the genus Candida. With the aid of sterile oral spacers, an oral sample was collected with sterile swab, seeded in petri dishes containing dextrose agar Sabouraud with added chloramphenicol, incubated at 25°C and examined in 24 and 48 hours. In patients who did not present lesions, samples were collected to investigate the presence of the yeast. The samples that showed the growth of creamy colonies in the culture and gram-positive yeast cells on direct microscopy were considered as positive results for yeasts of the genus Candida.
Variables and data analysisThe presence of Candida spp. was utilized as dependent variable, therefore including the patients who had candidiasis and those who had fungus of the genus Candida. For independent variables, data from the questionnaire applied to the patients were used.
All data were recorded and typed into a specific databank for the descriptive and inferential statistical analysis of this study. Data were electronically processed with the program Statistical Package for Social Science (SPSS), version 17.0. In the present study, we opted not to perform a multivariate analysis and to use a bivariate analysis with Pearson’s chi-square test (χ2). This is a test of hypotheses destined to find a value of the dispersion for two normal variables and to evaluate the existence association between qualitative variables. Therefore, the association between the dependent variable (presence of Candida spp.) And the independent variables were tested at a level of significance of 5% and a confidence interval of 95%, taking the unilateral hypothesis into consideration. The variables associated to the outcome were those that had a level of significance lower than 0.05.
ResultsData descriptive analysisOf the 49 individuals evaluated in this study, most were female (83.7%) with a mean age of 59 years, the majority married (87.8%) and living in the state of Rio Grande do Sul (83.3%). More than half of the participants (57.1%) were not practicing their occupation (inactive). Regarding the individual monthly income, 55.1% received up to R$ 2,000.00. The larger proportion of liver recipients underwent transplantation less than 10 years back (63.3%), according to table 1.
Total distribution of liver recipients according to sociodemographic variables
| Sociodemographic variables | n (49) | % (100) |
|---|---|---|
| Sex | ||
| Male | 8 | 16.3 |
| Female | 41 | 83.7 |
| Age group | ||
| 21 to 59 years | 24 | 49.0 |
| 60 to 78 years | 25 | 51.0 |
| Marital status | ||
| Married | 43 | 87.8 |
| Single, widowed, divorced | 6 | 12.2 |
| State | ||
| Rio Grande do Sul | 40 | 83.3 |
| Santa Catarina | 9 | 16.7 |
| Current professional activity | ||
| Active | 21 | 42.9 |
| Inactive | 28 | 57.1 |
| Individual monthly income | ||
| Up to R$ 1,000.00 | 13 | 26.5 |
| From R$ 1,000.00 to R$ 2,000.00 | 14 | 28.6 |
| Above R$ 2,000.00 | 22 | 44.9 |
| Date of the transplant | ||
| 1 to 9 years | 31 | 63.3 |
| 10 to 15 years | 18 | 36.7 |
Hepatitis C was the main condition that led to transplant, having affected 20 (41%) patients in the sample, followed by hepatitis B (29%), alcoholism (14%), cancer (6%) or other causes (10%).
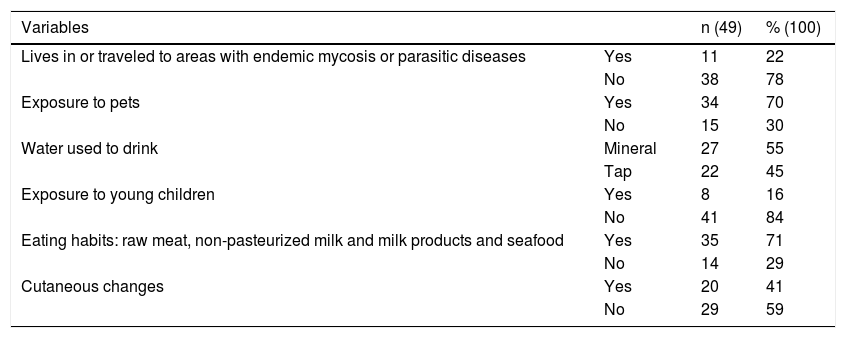
Regarding the variables related to environmental exposure, 38% reported living in or having traveled to areas out of their state of residency. Regarding dietary habits, 71% reported eating at least one of the following foods: raw meat, non-pasteurized milk and milk products and seafood. In addition, 27% drank mineral water and 41% reported cutaneous changes after the transplant (Table 2).
Distribution of the liver recipients regarding exposure to environmental factors and dietary habits
| Variables | n (49) | % (100) | |
|---|---|---|---|
| Lives in or traveled to areas with endemic mycosis or parasitic diseases | Yes | 11 | 22 |
| No | 38 | 78 | |
| Exposure to pets | Yes | 34 | 70 |
| No | 15 | 30 | |
| Water used to drink | Mineral | 27 | 55 |
| Tap | 22 | 45 | |
| Exposure to young children | Yes | 8 | 16 |
| No | 41 | 84 | |
| Eating habits: raw meat, non-pasteurized milk and milk products and seafood | Yes | 35 | 71 |
| No | 14 | 29 | |
| Cutaneous changes | Yes | 20 | 41 |
| No | 29 | 59 |
Of the 49 patients evaluated, the presence of Candida spp. was seen in 19 (39%) and of those, six (12%) had oral candidiasis, four (66%) of the atrophic type and two (33%) of the pseudomembranous type (Figure 1 and Figure 2).
Of the 19 (39%) samples of Candida, eight (42%) were C. albicans, confirmed by the formation of the germ tube and 11 (58%)Candida non-albicans.
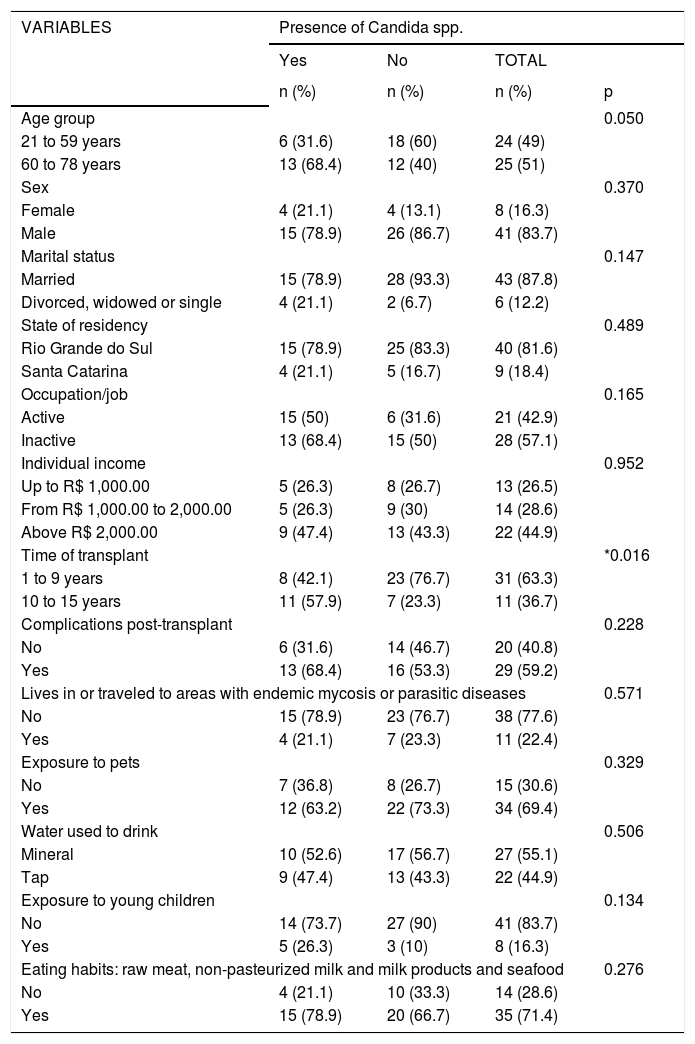
Data inferential analysisAfter the statistical analysis, it was possible to observe that regarding the sociodemographic characteristics, the variable time from transplant was associated to the dependent variable of presence of Candida spp. This result shows an increased presence of Candida spp. in patients with a longer time from transplant (p = 0.016). Regarding the variable age group, there were no relationships between the variables, however, the values were borderline with p = 0.05. The results are shown in table 3.
Inferential analysis between the dependent variable presence of Candida spp. and independent variables
| VARIABLES | Presence of Candida spp. | |||
|---|---|---|---|---|
| Yes | No | TOTAL | ||
| n (%) | n (%) | n (%) | p | |
| Age group | 0.050 | |||
| 21 to 59 years | 6 (31.6) | 18 (60) | 24 (49) | |
| 60 to 78 years | 13 (68.4) | 12 (40) | 25 (51) | |
| Sex | 0.370 | |||
| Female | 4 (21.1) | 4 (13.1) | 8 (16.3) | |
| Male | 15 (78.9) | 26 (86.7) | 41 (83.7) | |
| Marital status | 0.147 | |||
| Married | 15 (78.9) | 28 (93.3) | 43 (87.8) | |
| Divorced, widowed or single | 4 (21.1) | 2 (6.7) | 6 (12.2) | |
| State of residency | 0.489 | |||
| Rio Grande do Sul | 15 (78.9) | 25 (83.3) | 40 (81.6) | |
| Santa Catarina | 4 (21.1) | 5 (16.7) | 9 (18.4) | |
| Occupation/job | 0.165 | |||
| Active | 15 (50) | 6 (31.6) | 21 (42.9) | |
| Inactive | 13 (68.4) | 15 (50) | 28 (57.1) | |
| Individual income | 0.952 | |||
| Up to R$ 1,000.00 | 5 (26.3) | 8 (26.7) | 13 (26.5) | |
| From R$ 1,000.00 to 2,000.00 | 5 (26.3) | 9 (30) | 14 (28.6) | |
| Above R$ 2,000.00 | 9 (47.4) | 13 (43.3) | 22 (44.9) | |
| Time of transplant | *0.016 | |||
| 1 to 9 years | 8 (42.1) | 23 (76.7) | 31 (63.3) | |
| 10 to 15 years | 11 (57.9) | 7 (23.3) | 11 (36.7) | |
| Complications post-transplant | 0.228 | |||
| No | 6 (31.6) | 14 (46.7) | 20 (40.8) | |
| Yes | 13 (68.4) | 16 (53.3) | 29 (59.2) | |
| Lives in or traveled to areas with endemic mycosis or parasitic diseases | 0.571 | |||
| No | 15 (78.9) | 23 (76.7) | 38 (77.6) | |
| Yes | 4 (21.1) | 7 (23.3) | 11 (22.4) | |
| Exposure to pets | 0.329 | |||
| No | 7 (36.8) | 8 (26.7) | 15 (30.6) | |
| Yes | 12 (63.2) | 22 (73.3) | 34 (69.4) | |
| Water used to drink | 0.506 | |||
| Mineral | 10 (52.6) | 17 (56.7) | 27 (55.1) | |
| Tap | 9 (47.4) | 13 (43.3) | 22 (44.9) | |
| Exposure to young children | 0.134 | |||
| No | 14 (73.7) | 27 (90) | 41 (83.7) | |
| Yes | 5 (26.3) | 3 (10) | 8 (16.3) | |
| Eating habits: raw meat, non-pasteurized milk and milk products and seafood | 0.276 | |||
| No | 4 (21.1) | 10 (33.3) | 14 (28.6) | |
| Yes | 15 (78.9) | 20 (66.7) | 35 (71.4) | |
Solid organ transplant recipients are under the risk of fungal infections, many times due to the prolonged use of immunosuppressive drugs. The knowledge of the fungal species, the early diagnosis and the adequate treatment of these infections are key to improve the survival and reduce the mortality of transplant patients.4 In this study we demonstrated a prevalence of presence of Candida spp. of 39%. Levesque et al.14 investigated 52 liver transplant patients in the hospital in France and found yeasts of the genus Candida in 81% of the individuals, C. glabrata being the most prevalent species (47%). The same study demonstrated that during the period of observation, six cases of invasive candidiasis occurred in these patients. A research conducted by Rai et al.15 demonstrated 29 positive samples for the presence of Candida, Aspergillus or Alternaria as agents of secondary infections out of a total of 45 samples collected from sick patients. Solid organ transplant recipients are susceptible to opportunistic infections, therefore the correct diagnosis and the knowledge on the epidemiology of the main infectious fungus becomes important.16
Despite the lack of sufficient evidences to prove that liver transplant recipients have a higher prevalence of Candida spp. in the oral cavity compared to immunocompetent individuals, we can call attention for the need of specialized care with the oral cavity of these patients in order to avoid complications such as systemic infections caused by opportunistic microorganisms due to the use of immunosuppressive therapy after the transplant.
Infections by Candida species correspond to the larger part of invasive mycosis in the group of transplant patients.12 In this study we observed six (12%) cases of oral candidiasis, four (66%) of the atrophic type and two (33%) of the pseudomembranous type. A similar study was performed by Rojas et al.17, in which they reported a rate of 7.5% of clinical candidiasis in liver transplant recipients. In a study conducted by Gondim et al.18, the prevalence of candidiasis ranged from 3.7% to 18.7%, with the erythematous (atrophic) type being the most frequent. Rezvani et al.19 observed oral candidiasis of the erythematous type in 8.5% of the patients studied (immunosuppressed transplant recipients) and also found a percentage of 17.1% of episodes of candidiasis, with 76% of the pseudomembranous type. In another study with kidney transplant patients, 15.8% had oral candidiasis.20
These facts demonstrate that immunosuppressed patients are more vulnerable for the development of candidiasis because, despite the occurrence of infectious episodes between many studies being variable, they are more frequent in solid organ recipients.
Even though multiple studies demonstrate C. albicans as the main species isolated from patients with invasive candidiasis, we can observe a significant increase in Candida non-albicans species, particularly C. tropicalis andC. parapsilosis, and that tendency has already been noted in any situations of candidemia.21 In this study, eight species of C. albicans and 12 of Candida non-albicans were identified. A study performed by Levesque et al.14 reported 42 cultures (81%) of Candida spp., with the prevalent species being C. glabrata (47%), what demonstrates the importance of the identification of the fungal species, since Candida non-albicans species can present with a reduced sensitivity to certain conventional antifungals. In contrast to this study, the investigation conducted by Mímica et al.22 characterized 50% of the samples as C. albicans; 20.8%, C. tropicalis; 2.4%, C. krusei and 26.9%, other species (undetermined). Crocco et al.23, identified with the CHROMagar Candida technique, C. albicans in 76% of the studied samples, C. krusei in 19%, followed by C. tropicalis in 1%. Also, in Rocha et al.24research, C. albicans was the most prevalent species (86.4%), followed by C. tropicalis (4.5%). In the study by Wingeter et al.25, 93% de C. albicans were identified in the samples. These studies highlight the importance of the identification of the fungal agent in order to indicate the adequate treatment as early as possible, avoiding the risk of invasive fungal infections.26
Oral candidiasis can be considered a problem that aggravates the health of individuals with an abnormality of the immune system due to the use of immunosuppressants.21 In this study, the presence of the disease was compared to variables subjected to possible risk factors. After statistical analysis, we found that the time of the transplant was associated to the dependent variable of presence of candidiasis. In a similar study, Couto et al.27 observed that the fungal infection in patients submitted to liver transplant is dependent on some factors that can interact favoring the appearance of the disease, such as intensity of exposure to potential pathogens, degree of immunosuppression used and post-operatory care. Sun et al.28 observed that age and frequency of daily brushing of the teeth were risk factors for colonization by Candida spp., even though there was no significant relationship with the patient’s age in this study, but the values were close to significant. Regardless of the type of transplant and immunosuppressant drugs, studies highlight attention with possible risk factors, because these require different strategies for the prevention and control of Candida spp. infection.
As limitations of this study, we can report the small sample seen at the ambulatory of the hospital in the period of the study, the inclusion of patients in different stages of immunosuppression as well as the absence of a healthy control group, which hindered a design that allowed comparing between groups. This way, it would have been possible to reach more definitive conclusions when comparing the results to those of other studies.
It is important to note the results of the study on the subject can be explained by different designs, diversity in sample sizes and indicators of evaluation, besides other factors that can also be involved.
Even though the sample size is small, the results highlight the need for a more effective control of the health of these patients, particularly those with more advanced age. Besides, there was a higher incidence of the presence of Candida spp. in patients with longer time of transplant, increasing the morbidity risk in this population.
ConclusionCandida species classified as non-albicans have been emerging in all fungal infections. This scenario is concerning, since the antifungal armamentarium available is very restricted and, in some cases, ineffective in infections caused by multiresistant strains. The infection reaches this severity when the correct diagnosis is not made due to the lack of laboratory standardization for the identification of fungi.
We demonstrate in the group studied that the oral cavity of liver transplant patients is being inhabited, in most part, by Candida non-albicans, what can be an alert for a more effective control of the health of these patients, particularly in those with more advanced age.
Financial support: None.
Conflict of interest: None.