A 37-year-old man complained of a refractory posterior malleolar ulceration on his left ankle. He was diagnosed with Werner syndrome according to the progeroid clinical features and genetic testing. To approach the ulceration, a free flow-through right anterolateral thigh perforator flap with anterolateral thigh cutaneous nerve was harvested. One year later, he was readmitted due to a new ulceration on his right ankle. We harvested the left anterolateral thigh perforator flap with anterolateral thigh cutaneous nerve to reconstruct the defect. After one more year of follow-up, there was no recurrence of ulcers, and the sensation of the flap recovered partially after 6 months. We conclude that free flow-through anterolateral thigh perforator flap is a feasible choice for the repair of foot ulcers in Werner syndrome.
Werner’s syndrome is a rare, autosomal recessive condition with multiple progeroid features. It was first described by Otto Werner in 1904.1 It is characterized by bilateral cataracts, premature graying, dermatologic changes and short stature, intractable skin ulcers, bird-like facies, and abnormal voice.2 Confirmation of a clinical diagnosis requires WRN gene testing.3
Although it is difficult to repair the cutaneous ulcers in Werner’s syndrome, their prevention or reduction of recurrence is extremely important. First, a definite diagnosis should be made. Incorrect diagnosis and inappropriate therapeutic regimen may increase the risk of amputations because of incurable ulceration. We report a typical case treated with contralateral innervated free flow-through anterolateral thigh (ALT) perforator flaps to repair ulcers on both heels. To our knowledge, this is the first report of this technique for the treatment of refractory ulcers in Werner syndrome.
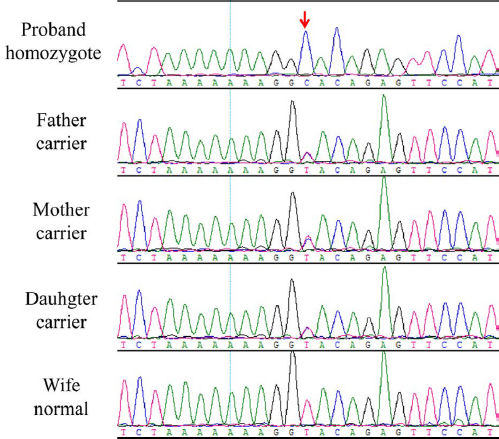
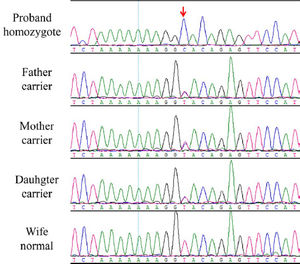
Case ReportA 37-year-old man was admitted for evaluation and treatment of skin ulcers on his left lower limb. The patient had depressed scars, epidermis fibrosis, and hyperpigmentation on both lower extremities. There was a family history of consanguineous marriage. The patient had no history of trauma or deep vein thrombosis. Physical examination revealed short stature (142cm) and body weight 37kg. The patient had slender extremities, prematurely gray hair, atrophy of the skin and subcutaneous tissue, beak-shaped nose, high-pitched voice, and juvenile cataracts. X-ray revealed calcification of the Achilles tendon. Doppler ultrasound showed moderate arteriosclerosis in both lower extremities. Genetic analysis revealed a homozygous mutation, a T to C substitution at the splice site of intron 28 of WRN gene (IVS28+2C, Figure 1).
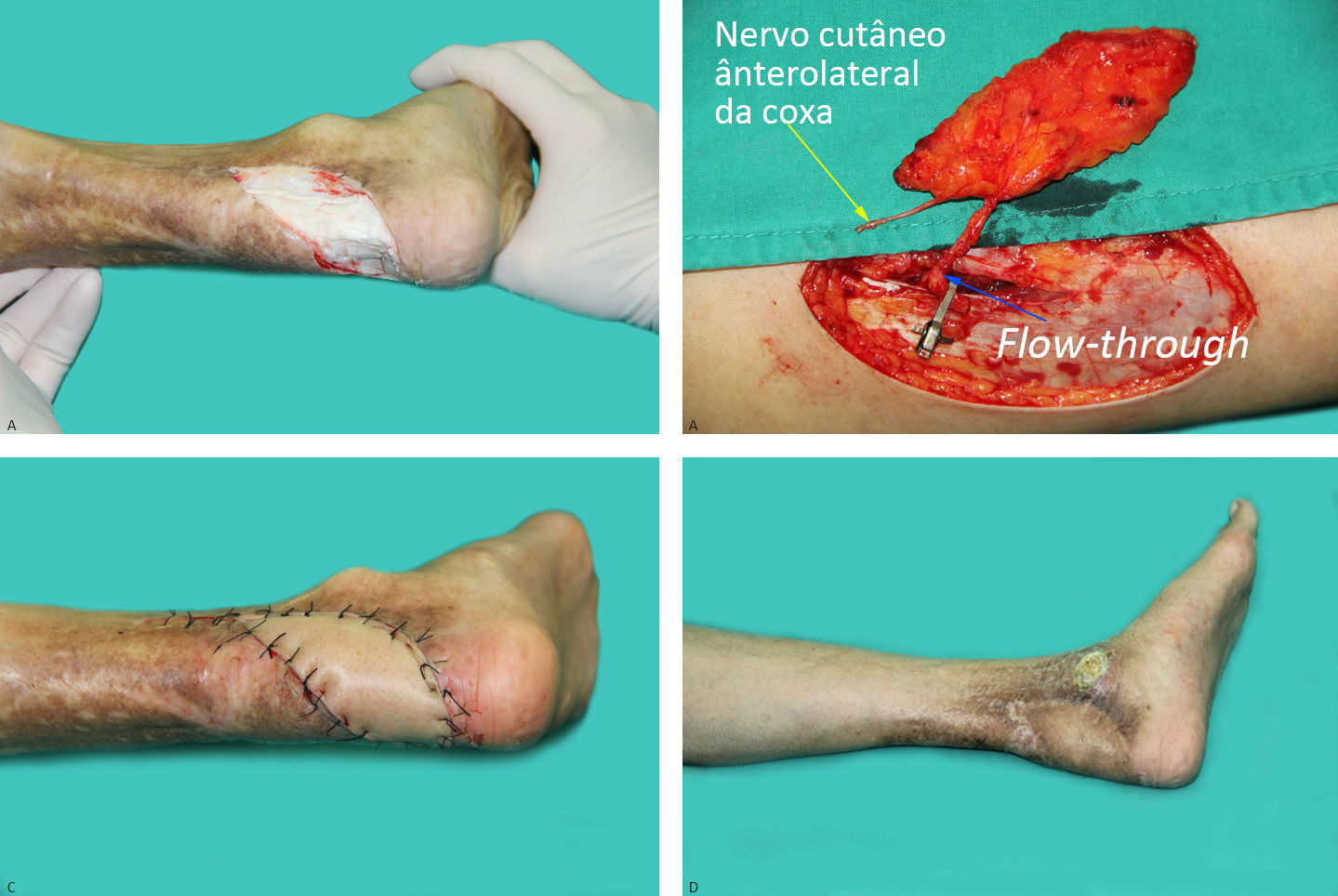
Previous local pedicle flap had been transferred to repair the ulcer, but the ulcer reccured and the Achilles tendon was exposed (Figure 2A). Because of the previous injury to local vessels and the poor blood supply to the distal foot due to arteriosclerosis, the decision was made to harvest a contralateral flow-through ALT perforator flap with anterolateral thigh cutaneous nerve (Figure 2B). After surgical debridement, we measured the size of the defect and dissected an ALT perforator flap on the right donor site. The flap was then transferred to the recipient site (Figure 2C). The proximal descending branch of lateral circumflex femoral artery was anastomosed to the proximal posterior tibial artery, and the distal branch was anastomosed to the distal posterior tibial artery. The two veins of the flap were respectively anastomosed to two veins accompanied with the posterior tibial artery. Finally, the anterolateral femoral cutaneous nerve was coaptated to the recipient medial calcaneal nerve. The flap survived and recovered protective sensation at 12 months’ follow-up (Figure 2D).
However, the patient complained of a right posterior malleolar ulceration after one year and was readmitted (Figure 3A). After adequate debridement, a contralateral free flow-through ALT perforator flap was designed to cover the defect (Figure 3B). Vascular anastomosis method was similar as before. The postoperative care was uneventful. So far there has been no further development of ulcer on either heel, only inconspicuous linear scars in the donor site (Figure 3C and 3D).
DiscussionWerner’s syndrome is usually accompanied by metabolic abnormalities in the connective tissue, arteriosclerosis, diabetes, ectopic calcification, and atrophy of the subcutaneous tissue and muscle.4 Ulcer in the extremity is one of the most difficult clinical problems in patients with Werner’s syndrome.5 Thus, seeking an effective method to repair this specific ulceration is highly significant.
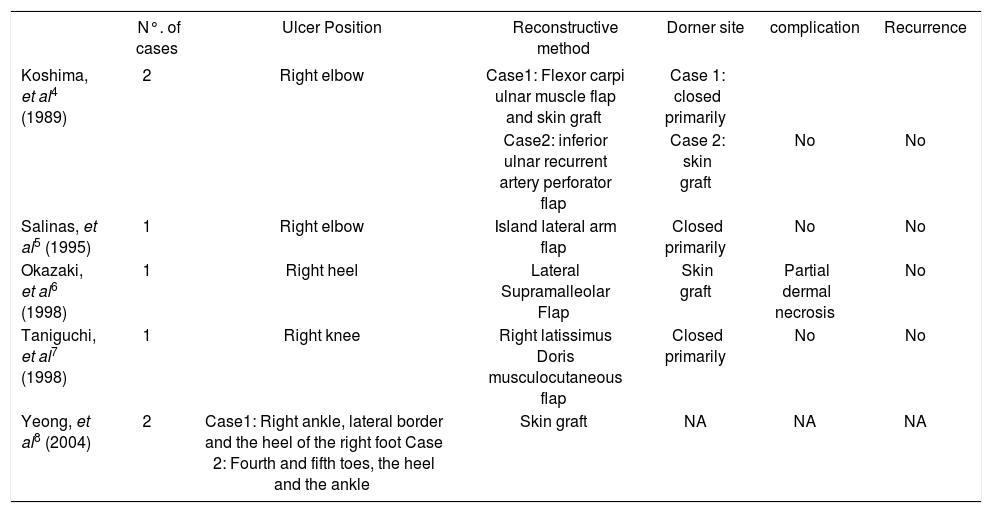
Numerous studies have reported different methods to repair ulcers (Chart 1).6-10 First, skin grafting is not recommended. Due to the poor blood supply to the ulcer base, a skin graft does not easily survive. Even if the grafted skin survives, the ulcer is hardly resistant and easily relapses. Second, local pedicle flaps are not useful for the treatment of intractable ulcers of the extremities because of scleroderma-like skin lesions and poor blood supply. Our patient had failed to heal the wound with a local pedicle flap. It is thus advisable to carefully assess the patient’s general clinical status before surgery if one chooses a pedicle flap. Third, muscle or musculocutaneous flaps, including flexor carpi ulnar muscle flap and latissimus dorsi flap, should be used with caution in the Werner’s syndrome patient because of the functional loss at the donor site. Moreover, the musculocutaneous flap is bulky and unable to carry the nerve to reconstruct sensation.
Various methods for treating ulcers in Werner syndrome
| N°. of cases | Ulcer Position | Reconstructive method | Dorner site | complication | Recurrence | |
|---|---|---|---|---|---|---|
| Koshima, et al4 (1989) | 2 | Right elbow | Case1: Flexor carpi ulnar muscle flap and skin graft | Case 1: closed primarily | ||
| Case2: inferior ulnar recurrent artery perforator flap | Case 2: skin graft | No | No | |||
| Salinas, et al5 (1995) | 1 | Right elbow | Island lateral arm flap | Closed primarily | No | No |
| Okazaki, et al6 (1998) | 1 | Right heel | Lateral Supramalleolar Flap | Skin graft | Partial dermal necrosis | No |
| Taniguchi, et al7 (1998) | 1 | Right knee | Right latissimus Doris musculocutaneous flap | Closed primarily | No | No |
| Yeong, et al8 (2004) | 2 | Case1: Right ankle, lateral border and the heel of the right foot Case 2: Fourth and fifth toes, the heel and the ankle | Skin graft | NA | NA | NA |
NA = not available or unknown from literature.
We thus use contralateral free flow-through ALT perforator flaps with anterolateral femoral cutaneous nerves for the repair of heel ulcer in Werner syndrome. There are numerous advantages: (1) Flow-through technique enables the vascular pedicle to maintain dual blood supply of flap and distal extremity. (2) In Werner syndrome, it is suitable to repair limb ulcers with ALT flaps owing to lipoatrophy of the thigh. Our patient’s fat thickness was 8mm, and the recipient site developed a satisfactory appearance. (3) Patients with Werner’s syndrome have arteriosclerosis, so sacrificing major vessels should be avoided if possible, because it can cause irreversible damage to circulation in the lower leg in the future. A flow-through ALT perforator flap with the lateral femoral cutaneous nerve not only handily bridges the posterior tibial artery but also acquires partial sensation. (4) With protective sensation, the patient can wear shoes and walk normally. (5) The donor site was closed primarily in this case, and only linear scars were left at the donor site.
We conclude that contralateral free flow-through ALT perforator flap is a feasible choice for repair of heel defects in patients with Werner syndrome. The anterolateral thigh cutaneous nerve can be transferred with the flap to recover protective sensation.
Financial support: National Natural Science Foundation of China (81472104).
Conflict of interest: None.