Dear Editor,
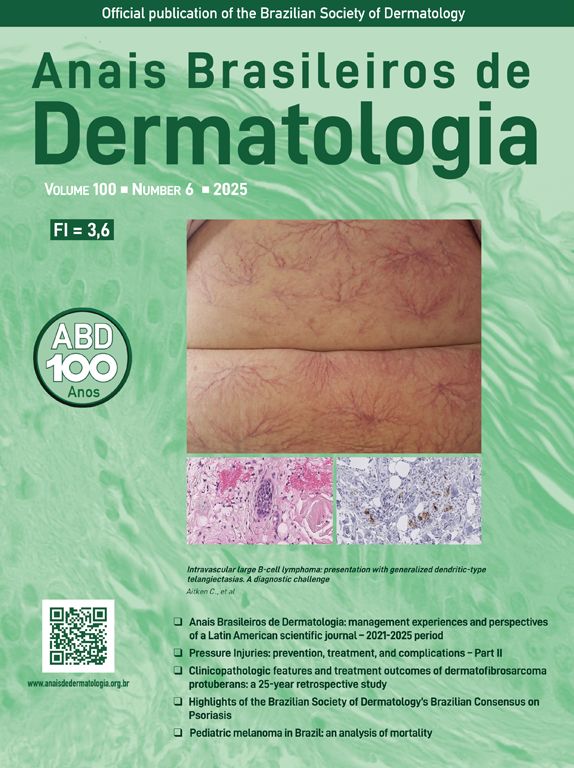
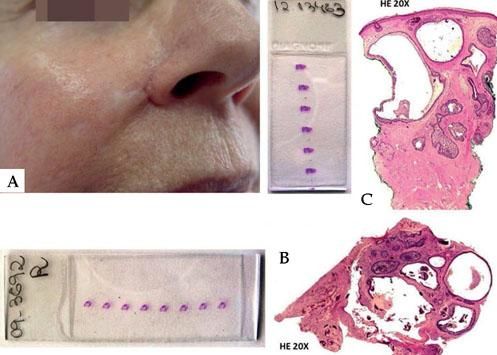
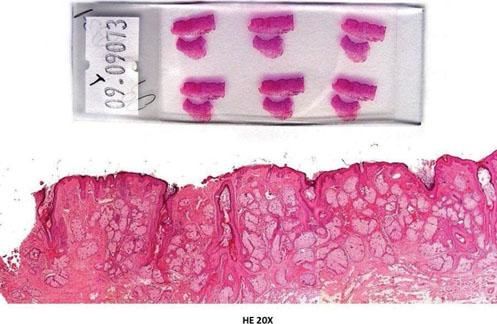
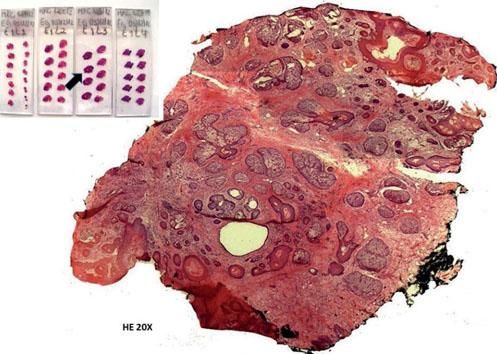
Reports indicating "absence of residual neoplasm" are not uncommon in cases of reoperation of patients where the initial resection was incomplete. This usually leads to the conclusion that the tumor had been completely removed, which can be misleading and could be complicated to prove that the operation was not performed on the wrong site.1 This case exemplifies this situation and points out the importance of demonstrating the residual tumor. In 2012, a 75-year-old female patient was referred to the clinic with a suspected recurrence of a basal cell carcinoma located in the nasolabial sulcus next to the right nasal ala that had been operated in 2009 (Figure 1A). In 2009, a punch biopsy was performed and the histopathology report revealed an adenoid basal cell carcinoma (Figure 1B). The patient was referred to a plastic surgeon in 2009. The surgery report revealed "solar keratosis and a small focus suggestive of basaloid proliferation" (Figure 2). The plastic surgeon considered the case "closed". In 2012, a new punch biopsy at the same site showed the same histopathological findings as the first biopsy in 2009, demonstrating the persistence of the tumor (Figure 1C). A micrographic surgery using the three-dimensional method was able to detect a small amount of residual basal cell carcinoma, which was located eccentrically in the surgical specimen and showed tumor-free surgical margins after the first stage, the same histological pattern found in 2009 (Figure 3). Therefore, it was possible to demonstrate that the tumor was recurrent and it was totally excised. It could be misleading to claim a case as "solved" after a surgery report that indicates tumor-free margins as one must be aware of how relative histopathology reports can be, especially when less than 1% of the total surgical margin is examined.2 Effectiveness of surgeries that remove neoplasms can only be properly tested by the absence of further clinical manifestations. However, if clinical symptoms arise, it is difficult to determine if they represent a new tumor or if they are related to the previous tumor. Finding the residual tumor with actual tumor-free margins in the final, definitive surgery is a good sign that the surgery was effective. Failure to detect the residual tumor is quite unexpected and some will mistakenly interpret it as a sign of spontaneous regression or as the surgeon's incredible ability to have cauterized the proper vessel and accurately electrocoagula-ted what remained of the tumor.3 Perhaps the best explanation for not finding the residual tumor is the fact that in routine tests only tiny samples of the surgical specimen are examined. The smaller the mass of the remaining tumor, less likely is its detection.4 Likewise, the assertion that microscopically controlled surgeries always solve the dilemma of compromised margins should be reviewed, especially when dealing with forms of peripheral microscopic control. In this case, no neoplastic tissue would be identified if the surgery had only one stage. The so-called "debulking" can be obtained differently depending on the surgeon: while some will curette the initial tumor or the area to be operated, others will remove the visible part of the tumor or the area to be operated and examine it in paraffin. Again, with small samples the residual tumor may go unnoticed. Thus, there is no difference between conventional surgery and microscopically controlled surgery (peripheral type) when only one stage is performed, since they were equally incapable of detecting the residual tumor. Consequently, they are unable to prove that the surgery was not performed on the wrong site.5 The clinical-surgical case described shows how the residual tumor is important to understand the outcome as it demonstrates facts that explain what may have occurred and certifies that all the surgical margins were free. Any new local clinical manifestation can be accurately interpreted as the appearance of a new tumor and not as a recurrence.
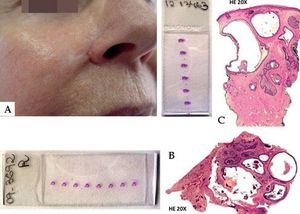
A - Punch biopsy performed in 2012 in the scarred area located near the right nasal ala. Patient had been biopsied and operated on the same site in 2009, when the problem was allegedly solved. B - Slide and corresponding histology of the punch biopsy performed in 2009 in the area located near the right nasal ala (Hematoxylin & eosin, x20). C - Slide and corresponding histology of the punch biopsy performed in 2012 in the same region. Histopathological findings are identical and confirm the persistence of the tumor (Hematoxylin & eosin, x20)
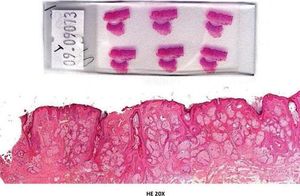
Slide and corresponding histology of the surgery performed by a plastic surgeon in 2009 who supposedly operated on the correct site. Although the report issued by another laboratory revealed a small focus suggestive of basaloid proliferation, nothing is observed in the histological section that may resemble the tumor pattern evidenced in the biopsies (Hematoxylin & eosin, x20)
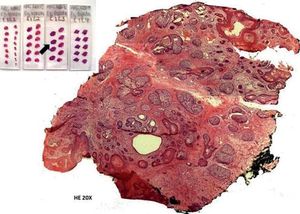
Slides and histological section of the micrographic surgery (Munich method). The tumor appears on the first three sections of slide 3 and persists througout the end without compromising the margins. The histological picture shows the cut 3 in the slide 3 (arrow) where the same histological pattern found from the biopsy can be observed. The residual tumor is not found in the center of the specimen. An ordinary sample might not have caught the tumor, neither would micrographic methods that examined only the surgical border (Hematoxylin & eosin, x20)