Dear editor,
The nevus lipomatosus cutaneous superficialis (NLCS) is a rare benign hamartomatous tumor.1–3 It presents in two clinical forms: the classic and the solitary. The classic form usually occurs in childhood and adolescence and is characterized by multiple asymptomatic, soft, cerebriform, pedunculated, yellow or skin-colored papules, nodules or plaques.3 The solitary form is uncommon and usually affects individuals older than 20 years of age; it presents as a single sessile papule or dome-shaped lesion.1
The treatment option is usually motivated by cosmetic purposes, because there are no systemic consequences nor associated malignant tumors. Surgical excision is an appropriate option if the patient decides to treat.1,4 We report an unusual case of classic NLCS, with onset in an atypical age group that had satisfactory clinical response with topical corticosteroid treatment.
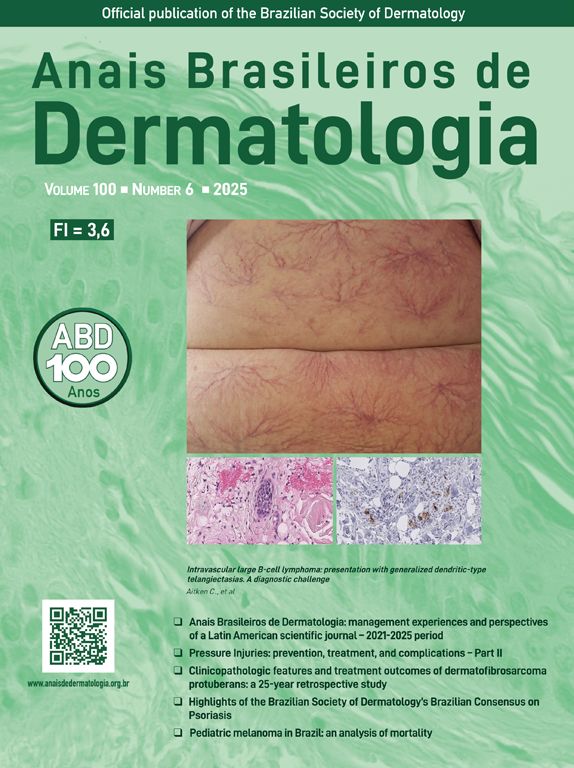
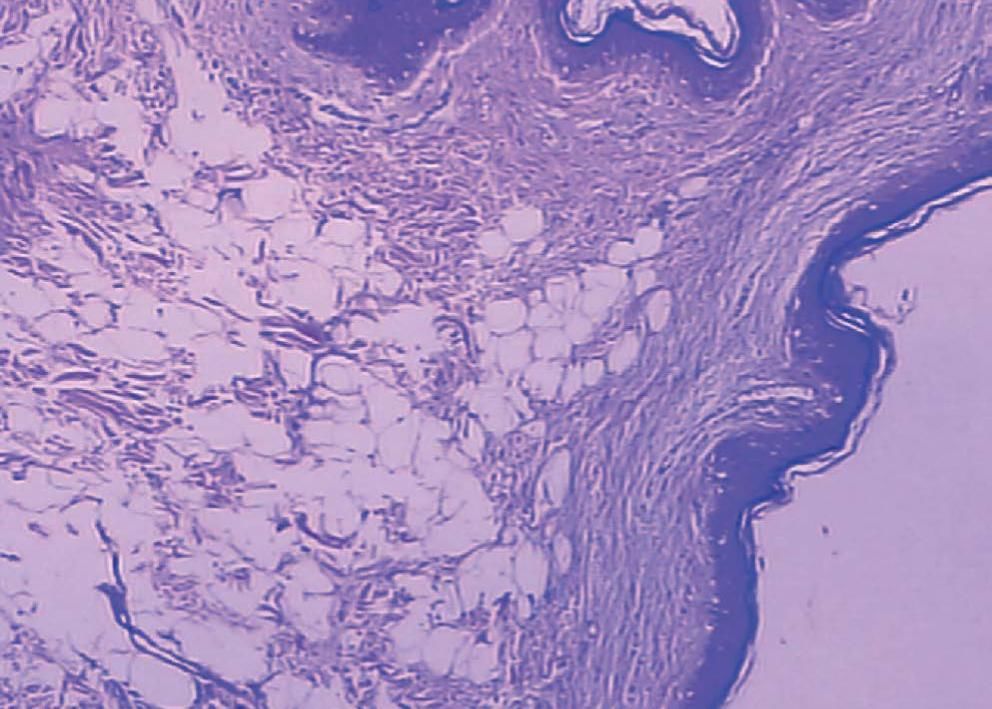
Female, 52-year-old patient, smoker, presented with the lesion on the back for almost 2 years. In hot days and with sun exposure, the lesion became itchy with development of erythema and edema. Physical examination revealed a yellow plaque formed by multiple pedunculated and confluent papules, measuring 7 cm x 10 cm, on the right infrascapular region, following the Blaschko’s lines, not crossing the median line (Figure 1). Darier sign was negative. Initial differential diagnosis were solitary mastocytoma, neurofibroma, cutaneous leiomyoma and Shagreen patch. A punch n.º 4 biopsy was performed and the histopathology revealed mast cells in the subtle superficial and interstitial perivascular inflammatory infiltrate, suggestive of cutaneous mastocytosis. We prescribed fludroxycortide (0.125 mg/g) cream whenever the lesion became itchy. The patient used the medication almost daily for four months, with improvement of the symptoms and partial involution of the lesion (Figure 2). Despite worsening with heat and sun exposure, the clinical aspect and the course of the lesion were not typical of cutaneous mastocytosis, so we suspected NLCS. A new incisional biopsy was performed (ellipse) and the histopathology revealed mature fax tissue in the dermis, more prominent around the vessels and associated to dermal perivascular and interstitial mast cells – findings there are consistent with NLCS (Figure 3). We opted not to perform surgery due to the regression of the lesion with topical corticosteroid treatment and the lack of symptoms.
NLCS was first described by Hoffmann and Zurhelle in 1921.1 It is a benign and idiopathic malformation, characterized by the presence of mature ectopic fat tissue among the collagen bundles in the dermis.4 Familial occurrence was not seen, and neither was gender predilection or association with other systemic conditions.2
There are two forms of NLCS: the classical form, described by Hoffmann and Zurhelle, and the soliand the solitary form, both with chronic and asymptomatic course.1,4 In the classical form, multiple papules are seen, coalescing into plaques, with a zosteriform, linear or segmental distribution. They are skin colored or yellow, soft or with a cerebriform surface, and can reach large dimensions. They are located on the upper thighs, buttocks and on the lumbar region, are usually unilateral and are present at birth or in the first 2 decades of life.2,3,5 The solitary form arises from 30 to 50 years of age and is characterized by an isolated sessile or dome-shaped papule on any part of the body surface, but predominantly on the lower trunk, knees, axillae, upper limbs, earlobes and scalp.4
The diagnosis is based on the clinical suspicion and confirmation by histopathology. The histopathology reveals mature ectopic adipocytes interspersed with collagen bundles and proliferating around the periadnexal adventitious dermis and perivascular area. The mature adipocytes proliferate in the reticular dermis and extend to the papillary dermis, without connecting to the subcutaneous fat tissue.2 When there is extensive ectopic build-up of the mature adipocytes in the dermis, the area between the end of the dermis and beginning of the subcutaneous tissue is not clear. Therefore, a larger sample of tissue was paramount in allowing a more precise demarcation by the pathologist.
Treatment is essentially aesthetic and surgical excision is an adequate option.1 Non-surgical treatment options include cryotherapy, CO2 ablative laser and intralesional injections of phosphatidylcholine and sodium deoxycholate, with satisfactory clinical and histologic response.2,3
We report a case of classic NLCS that developed in the 5th decade of life – unusual age group –, that evolved with pruritus, contrary to the commonly asymptomatic course of the lesion. There is no report of the use of topical corticosteroids for the treatment of NLCS in the literature. In the case reported, the lesion improved significantly from the symptoms and clinical aspect after using fludroxycortide.
The case reported brings a new conception in regards to the use of topical corticotherapy for NLCS cases, that needs more clarification, but that elicits the possibility of a new safe, effective and non-invasive treatment, that can be particularly useful for large lesions.
Financial support: None.
Conflict of interests: None.