Background: Exposure to UVR provides benefits related to vitamin D synthesis, but also causes harms, since UVB is considered a complete carcinogen. There is no definition of the level of sun exposure and the proportion of exposed body required for proper synthesis of vitamin D in the skin without causing it damage.
Objectives: This study aims to analyze the sun exposure index, vitamin D levels and clinical changes in the skin caused by constant sun exposure in the fishermen population.
Methods: It is a cross-sectional, observational and analytical study The sample consisted of fishermen and was calculated in 174 individuals. The questionnaire was applied, the dermatological examination was carried out and the examinations of calcidiol, parathyroid hormone, calcium and phosphorus were requested. Data were expressed as percentages. The comparative analysis was done through the Chi-square test, and the correlations were established through the Pearson's linear coefficient.
Results: We observed that there was vitamin D deficiency in a small part of the cases (11.46%), and the frequency of diagnosis of skin cancer was 2.7% of the cases surveyed.
Study limitations: The difficulty in categorizing the sun exposure index.
Conclusion: The fact that fishermen expose themselves to the sun chronically and have been exposed to the sun for more than 15 years, between 21 and 28 hours a week, and without photoprotection, were indicative factors for protection against vitamin D deficiency. Chronic exposure to sun and high vitamin levels D may be indicative of protection of this population against skin cancer.
The energy emitted by the sun is transmitted as electromagnetic waves that are classified according to their length or frequency of propagation. They are mainly composed by infrared, visible and ultraviolet radiations. This group of radiations is known as optical radiation. Ultraviolet radiation (UVR), how the interval of the electromagnetic spectrum between the wavelengths of 100nm and 400nm is known, is subdivided into ultraviolet C (UVC), between 100nm and 280nm; ultraviolet B (UVB), between 280nm and 315nm; and ultraviolet A (UVA), between 315nm and 400nm.1
The ultraviolet index (UVI) is a value scale related to the biologically active UVR flow, which induces the formation of erythema in human skin and aims to inform the population about UVR intensity. Based on this parameter, education about the appropriate use of some protection is possible.2
Exposure to UVR has psychological and physical benefits, particularly related to the synthesis of vitamin D (VD) and the prevention of conditions such as osteoporosis, type I diabetes, some types of cancer and autoimmune and cardiovascular diseases.3,4
When a UVB light photon reaches the skin, it photoisomerizes 7-dehydrocholesterol (7-DHC) to form pre-cholecalciferol (pre-vitamin D3), which is isomerized into cholecalciferol (vitamin D3). It is then transported to the liver and kidneys where it undergoes hydroxylation and is converted into calcidiol (25 (OH) D) and, subsequently, into calcitriol (1.25 (OH) D). This is the most active metabolite, responsible to stimulate calcium and phosphate absorption through the intestines. Hydroxylation in the kidneys is stimulated by the parathyroid hormone (PTH) and suppressed by phosphorus.5,6
The dosage of VD is estimated through 25 (OH) D, since this is the main circulating form, with a half-life of about 2 to 3 weeks. Its concentration in the serum has a close correlation with the findings of osteomalacia and rickets and with the cutaneous production or ingestion of VD, which accurately reflects the body's supply of this vitamin. Alternatively, the levels of VD can be established through the levels of PTH. Therefore, low values of VD are related to increased levels of PTH which characterizes abnormal calcium homeostasis and secondary hyperparathyroidism.7
Hypovitaminosis D occurs when serum concentrations of calcidiol 25 (OH) D are below 30ng/mL (75nmol/L). Serum concentrations below 20ng/mL (50nmol/L) are classified as VD deficiency; between 20 and 29ng/mL (50 and 74nmol/L), as insufficiency and between 30 and 100ng/mL (75 e 250nmol/L), as sufficiency.8
At the same time that it is beneficial to human health, solar exposure can also cause damage. UVB is the most damaging wavelength for keratinocyte DNA and is considered a complete carcinogen. This radiation is responsible for the sunburn response and photo carcinogenesis, which consists in the development of skin cancers induced by UVR. Most of these damages are caused by direct and indirect photosensitive reactions and induce DNA breakage and base damage, therefore being lethal and mutagenic.9,10
Because the skin is the most accessible human organ to sunlight, it suffers directly the undesirable effects caused by UVR which nowadays represents the main environmental risk factor for the development of actinic keratosis (AK), squamous cell carcinoma (SCC) and basal cell carcinoma (BCC).11,12
The influence of UVR depends on the skin color, which can be evaluated using the classification of Fitzpatrick. This classification determines the different phototypes according to the cutaneous reaction to sun exposure.13
Public health campaigns have been developed to improve the knowledge of the general population on the role of this radiation in the development of skin cancer; however, the positive effects mediated by UVB light as the activator of VD production were not properly considered in most of these campaigns.14
There is no definition of the level of sun exposure and proportion of exposed body needed for an adequate synthesis of VD in the skin without damaging it. These aspects are important for thorough characterization of this epidemiological situation and are important tools in the education, if needed, of when and how to intervene in the prevention of cancer and vitamin D deficiency.15
The municipality studied is situated by the Atlantic Ocean. In its territory there are three rivers, a large number of creeks and watercourses, mangrove forests, besides seven lagoons, being an ecosystem rich in fishes, crustaceans and shellfish.16 Due to these characteristics, its economic background is fishing, agriculture, and, lately, tourism. The city has a fishermen colony established in April 1975 that nowadays houses 315 fishermen registered with the Registro Geral de Pesca.
The mean workload in Brazil is 39.4 hours per week. It is estimated that people working outdoors such as fishermen can receive a dose of UV radiation of 6 to 8 times higher than people working indoors, what certainly puts them at risk for the development of skin cancer and raises the interest in assessing their level of VD. 17
In this context we observe the importance of analyzing the index of solar exposure, the levels of vitamin D and the clinical changes on the skin caused by constant solar exposure in the fishermen population of the municipality.
MethodsIt is a cross-sectional, observational and analytic study. It was approved by the ethics committee under the number 1.606.041. The sample was made by fishermen of the fishing colony of a city in the northeastern coast. According to the fishermen colony, there are 315 registered fishermen with the Registro Geral de Pesca (RGP) living in the study area. The sample was calculated in 174 individuals with the program OpenEpi®, available online, considering an anticipated frequency of 50% and the accuracy confidence interval of 95%. The selection was random using the registration number through a draw with the program Randomizelist.
The health agents conducted home visits with the aim of inviting those selected to participate in the research according to the inclusion and exclusion criteria, attending a meeting at the fishermen colony, where the project was explained and the consent form was read. Those who could not attend the meeting was scheduled to have a consultation with the doctor in charge, where the objectives of the research were explained in the consent form read.
Fishermen of both genders, older than 18 years of age and active in their occupation participated in the study. Individuals who did not agree to signing the consent form, those working night shifts and those under the effect of some medication used in the previous 24 hours or that had any limitation to undergo examination for blood collection were excluded. The individuals that presented some previously diagnosed condition that was associated to or that could influence the levels of vitamin D, such as malabsorption diseases, burns, liver disease, kidney disease and calcium metabolism diseases were also excluded.
A semi-structured questionnaire was applied, which contained identification data such as codified name to protect the identity, date of birth, gender, weight, height, body mass index (BMI) and time in the occupation, besides variables related to possible risk factors that interfered in the VD serum levels such as diet, supplementation of VD or calcium, sunscreen use, the presence of skin lesions, phototype and index of solar exposure.
Soon after the skin was assessed with inspection and palpation, what allowed the accurate classification of the eruptive elements. The dermatologist performed dermatoscopy to evaluate pigmented skin lesions, making it possible to accurately differentiate between melanocytic and non-melanocytic pigmented lesions, and many times differentiating between benign and malignant lesions. In the cases with suspected malignant lesions, biopsy and surgery for treatment and confirmation of the diagnosis were performed. In the cases of premalignant lesions, cryotherapy was used for their treatment.
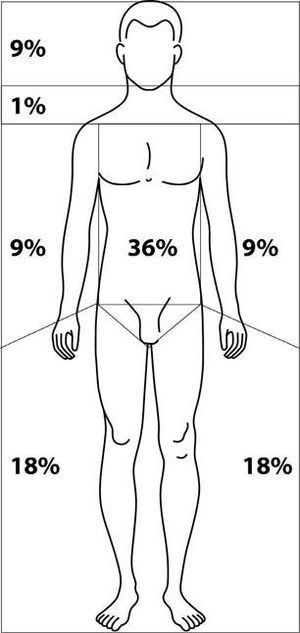
The analysis of sun exposure was made from the determination of the fraction of exposed area (FEA). It is calculated by dividing the body into multiples of nine in terms of site and time of sun exposure outdoors, and time of exposure (TE) to the sun per week, in amount of hours and minutes in which the body receives sun light (Figure 1 and Table 1). The index of solar exposure (ISE) was determined by multiplying TE by FEA.18
Fraction of the area exposed to the sun.
Source: Barger-Lux et al, 2002.18
Fraction of the area exposed to the sun
| Adaptation of the “rule of nines” | Category 1 | Category 2 | Category 3 | |||||
|---|---|---|---|---|---|---|---|---|
| No shirt | Long-sleeved shirt | Short-sleeved shirt | Shorts | Pants | No hat | With hat | ||
| 2 arms | 0.18 | 0.18 | 0.04 | 0.14 | ||||
| 2 legs | 0.36 | 0.24 | 0.00 | |||||
| Anterior trunk | 0.18 | 0.09 | 0.00 | 0.00 | 0.00 | 0.00 | ||
| Posterior trunk | 0.18 | 0.09 | 0.00 | 0.00 | 0.00 | 0.00 | ||
| Head | 0.09 | 0.07 | 0.03 | |||||
| Perineum | 0.01 | 0.00 | ||||||
| Total | 1.00 | 0.36 | 0.04 | 0.14 | 0.24 | 0.00 | 0.07 | 0.03 |
Source: Barger-Lux, et al, 2002.18
After applying the questionnaire, serum levels of calcidiol 25 (OH) D, PTH, calcium and phosphorus were requested. Biochemistry, calcium and phosphorus dosage were performed by calorimetry using the automated device A25 of the company Biosystems. The dosages of ionized calcium were performed by the technique of ion-selective electrode of the equipment AVL 9180. PTH dosage was performed by the technique of chemiluminescence with the automated device DXI from the company Backman; and that of 25(OH) D was performed by the technique of electrochemiluminescence with the automated device Modular E from the company Roche.
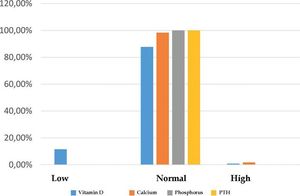
Were considered as reference levels: calcium: insufficiency <8.5mg/dl. sufficiency 8.5 to 10.8mg/dl and high >10.8mg/dl; phosphorus: insufficiency <2.5mg/dl, sufficiency 2.5 to 4.8mg/dl and high >4.8mg/dl; calcidiol (25(OH) D): deficiency <20ng/mL, insufficiency 21 - 29ng/mL, sufficiency 30 - 100ng/mL and high >100ng/mL; parathyroid hormone: insufficiency <15pg/mL, sufficiency 15 to 65pg/mL and high >65pg/mL.
The participants presenting any abnormalities in the blood tests were referred to the dietitian of the municipality to receive education on diet and to a dermatologist for supplementation of vitamin D.
The data obtained were expressed in percentages. The comparative analysis between the means of the groups was made with the Chi-square test. The correlations between the biochemical levels (serum levels of vitamin D, calcium, phosphorus and PTH), the time of solar exposure, the index of solar exposure and the skin lesions were established with the linear coefficient of Pearson. A significance of 5% (p<0.05) was considered. All analyses were performed using the software Genes.
ResultsThe sample had the following characteristics: 56.1% of males and 43.9% of females with no significant difference between the classes (x2=1.44; gl=1; p>0.05); the age ranged from 40 to 50 years in 35.46% of the sample; the time in the occupation was above 15 years for 54.72% of those interviewed (x2=50.07; gl= 3; p<0.01); 39.18% of the volunteers were overweight (x2 =79.69; gl= 5; p<0.01) and 72.9% did not report any associated conditions (x2=21.6; gl=7; p<0.01). Of those that had any condition, hypertension was the most common and was seen in 45% of the volunteers.
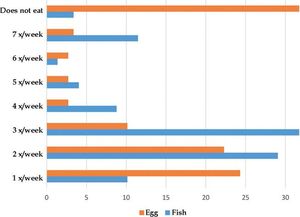
Among the food there are considered sources of VD we highlight fish and eggs. In the population studied, we observed that 31.75% ate fish three times a week (x2=78.67; gl=7; p<0.01) and the majority (31.75%) did not eat eggs (x2=78.67; gl=7; p<0.01) (Graph 1). Moreover, we also observed that almost all volunteers (95.27%) did not take any diet supplement (x2=81; gl=1; p<0.01) and 66.89% did not have the habit of drinking alcoholic drinks (x2=11.56; gl=1; 0<0.01).
Although the occupation demanded constant sun exposure, most of those interviewed (62.8%) did not use sunscreen; a small portion of 16.9% used it daily; and 20.3% used it occasionally (x2=39.44; gl=2; p<0.01). During dermatologic examination, no skin lesions were seen in 66.9% (x2=11.56; gl=1; p<0.01) of the volunteers. Among those who had lesions (33.1%), the diagnosis was divided into those who had skin cancer (8.2%) and those with precancerous/actinic keratosis (8.2%) and other types of skin lesions (83.6%) (x2=36.89; gl=2; p<0.01). Among other types of lesions the most frequent were pityriasis versicolor (25%) and seborrheic dermatitis (17.5%).
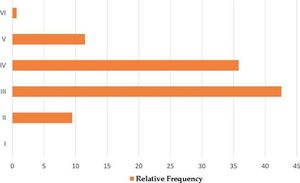
Graph 2 shows the phototype distribution of the volunteers in the study: we observed that 42.56% of the volunteers had phototype III and 35.81% phototype IV (x2= 98.8; gl=5; p<0.01) (Graph 2). Daily sun exposure was a constant and occurred in 91.83% of the fishermen (x2=70.56; gl=1; p<0.01). The index of sun exposure most commonly found in the group (49.65%) was that of from 0.1 to 10 (x2=44.96; gl=3; p<0.01).
There was vitamin D deficiency in a small portion of the cases (11.46%) with most results (87.7%) showing levels of 25 (OH) D above 30ng/mL (x2=210.76; gl=3; p<0.01). The levels of calcium were normal in 98.34% and high in 1.66% of those in the study. Phosphorus and PTH were within the normal range in 100% of the cases (Graph 3).
According to the Pearson's linear correlation test, a correlation between the variables studied was not observed, except for the variables regarding the use and frequency of use of sunscreen with r=0.7; p<0.05 (Table 2).
Estimation of the Pearson's coefficient of correlation between the variables studied
| TOcc | UProt | ATP | Lesion | SEI | Photot | VitD | Ca | P | PTH | |
|---|---|---|---|---|---|---|---|---|---|---|
| BMI | −0,045 | 0,145 | 0,156 | 0,197 | 0,153 | 0,155 | −0,068 | 0,003 | −0,120 | −0,062 |
| TOcc | - | −0,238 | −0,023 | 0,037 | −0,090 | −0,129 | 0,191 | −0,201 | 0,009 | 0,059 |
| UProt | - | - | 0,705* | −0,073 | −0,013 | 0,133 | 0,001 | 0,013 | −0,154 | 0,033 |
| ATP | - | - | - | −0,030 | 0,082 | 0,071 | 0,096 | −0,055 | −0,096 | 0,001 |
| Lesion | - | - | - | - | 0,108 | 0,114 | 0,049 | −0,036 | −0,018 | 0,011 |
| SEI | - | - | - | - | - | 0,202 | −0,068 | −0,018 | 0,030 | −0,218 |
| Photot | - | - | - | - | - | - | 0,022 | −0,075 | −0,029 | −0,230 |
| VitD | - | - | - | - | - | - | - | 0,064 | 0,015 | 0,115 |
| Ca | - | - | - | - | - | - | - | - | 0,104 | 0,028 |
| P | - | - | - | - | - | - | - | - | - | −0,117 |
BMI= body mass index; TOcc = time of occupation; Uprot = use of sun protection; ATP = amount of time using sunscreen; lesion = skin lesion; SEI = solar exposure index; Photot = phototype; VitD = vitamin D; Ca = calcium, P = phosphorus, PTH = parathyroid hormone
*Significant at 1% by T test
The geographical location of the municipality of the study is latitude 09059'08" and longitude 36021'03'', with a rainy tropical climate and dry summer.19 Due to these characteristics, the UVI levels are usually high. This represents very intense (UVI between 8 and 10) or extreme (UVI above 11) damage to human health.19 These levels can be seen even before 9 AM, throughout the year.20
Most fishermen in the sample ranged between 30 and 50 years in age, had phototype III and IV and were performing the occupation for over than 15 years. These data are the same found by Bezerra (2011) who, in his study with fishermen, found a mean age of 46.3 ± 9.54 years, ranging from 30 and 60 years. Predominance of phototype IV and mean time in the occupation of 29 ± 10.3 years, ranging from 12 and 45 years.21
BMI is used in epidemiological studies as an initial approximation of tendency of obesity in populations. The most commonly found BMI and the sample was between 25.0–29.9 and 39.18% of the volunteers, what represents excessive weight; however, in the study where the level of satisfaction with the body image was assessed, obesity and physical activity indicators in a fishermen village in Ceará, the BMI indexes shown for the total sample were 22.6 ± 2.3kg/m2, revealing that the sample is within the acceptable range.22
When asked, 72.97% of those in the study had no associated diseases. Between those who had, the most common was hypertension in a frequency of 45% of the volunteers. Studies performed showed that fishermen have a high prevalence of self-reported medical conditions, high prevalence of self-medication, poor diets and frequently smoked.23 The main health complaints were related to the musculoskeletal system, respiratory diseases, digestive system and ocular diseases, besides auditory problems.
Alcohol consumption was little seen in the sample studied. We observed that 66.9% of those in the study did not drink alcoholic drinks and only 2% drank them daily. These data disagree with a study performed in 2010 in a French fishermen and sailor population where it was observed that the daily consumption of alcohol was significantly higher among fishermen than in sailors (52.4g/day, 95% CI = 49.3–55.4 vs. 44.8g/day, 95% CI = 43.0– 46.6; p = 0.0003).24
Even though 91.83% of the fishermen in the study exposed daily to the sun, 62.83% of them did not use sunscreen. These data were the same found in the research conducted with beach workers, in which 85.4% frequently worked exposed to the sun but 61.3% did not use sunscreen.25
The skin lesions found among those interviewed (33.1%) were divided into those not related to sun exposure (83.6%) and those related to UVR (16.4%). One article relates the prolonged exposure of fishermen and other workers under the sun in their work environment with skin conditions caused by ultraviolet radiation.26 The authors defend the need for primary prevention in those workers against the effects of ultraviolet rays, particularly in those with less pigmented skin.
The skin lesions related to UVR researched in the sample were the precancerous ones, represented by actinic keratosis, found in a frequency of 2.7%, actinic cheilitis, 0% and by malignant skin tumors such as basal cell carcinoma (2.7%) and squamous cell carcinoma (0%). These data are partially compatible to the study, whose objective was to evaluate the role of general practitioners in selecting the population, mainly made by fishermen and farmers in the city in the north of Portugal, in which thorough skin examination by a dermatologist revealed 31% of actinic keratosis, 5% of leuco-plakia, 7% of basal cell carcinoma, 8% of squamous cell carcinoma, and 1% of melanoma.27 Similar data were observed in a previous study conducted in another coastal city of northeastern Brazil where clinically no cases of actinic keratosis or cutaneous neoplasms were diagnosed in the participants of the study.21
The frequency of skin cancer in fishermen and sailors has decreased over the last years. Among the reasons for this reduction we highlight the lower number of workers in these occupations, changes in work shift (night) and the use of sunscreen. However, in Brazil, skin cancer is the most frequent and corresponds to 30% of all malignant tumors registered in the country.28 In this study, all fishermen working at night were excluded and most volunteers did not use sunscreen, therefore, not explaining the low frequency of skin cancer in the sample studied.
There are many reasons that can explain the low incidence of skin cancer in this research. Among them we highlight: age over 40 years, low phototypes and constant sun exposure.
BCC is the most frequent of the epithelial malignant neoplasms and represents 65% of the total. It generally occurs in individuals older than 40 years.29,30 The sample of this study was made by 35.46% of the population aged between 40 and 50 years. Of the cases diagnosed with skin cancer the sample, all had BCCs, 25% of the patients were aged between 40–50 years, 50% between 50–60 and 25% were older than 60 years.
SCC frequency is of around 20% of the nonmelanoma skin cancers (NMSC) and it generally occurs in more advanced ages-after 50 years. These characteristics can explain the absence of diagnosis of this type of epithelial neoplasms among those in the study, since most volunteers were younger than 50 years.
Skin cancer is caused by sun exposure and its incidence rate is higher in lighter skin, sensitive to the sun.31 Among the 2.7% of cases diagnosed with BCC, 50% had phototype III and 50% had phototype IV. Of the individuals in the research, most were classified in the intermediate phototypes, of which 42.56% had phototype III and 35.81%, phototype IV. Therefore, individuals with that skin type have a lower incidence of cancer when compared to lower phototypes, that burn more easily than tan. Maybe for this reason there was a low number of skin cancer cases in the population studied.
Daily sun exposure was constant in the study and occurred and 91.83% of the cases. The explanation for a low frequency of NMSC in the fishermen can be due to the fact that chronic sun exposure leads to skin changes, that represent a defense mechanism with increasing the number of cell layers in the epidermis between the rete ridges and also melanocytes, besides not causing cutaneous immunosuppression, differently to the acute exposure to UVR.21
Vitamin D deficiency was diagnosed in 11.47% of the patients studied. This datum is not in agreement with the literature, since vitamin D deficiency is currently a worldwide public health problem in all age groups. According to the mapping performed, there was a prevalence of 77% of VD lower than 30ng/mL in individual studies conducted with adults in Brazil.32 In these studies, the prevalence of vitamin D deficiency (25(OH)D <29ng/mL) is between 33% to 71.2% in Brazil.33–36
The population older than 60 years of age in the sample of this study was 0.7% and this characteristic could have contributed to a low frequency of vitamin D deficiency, since the elderly are more prone to developing this deficiency because they expose less to UVR, have a reduced ability of cutaneous production, have inadequate diets and use many medications that can interfere with VD metabolism.37,38
BMI is another datum that could have contributed to the low frequency of vitamin D deficiency among those studied, because only 2.7% were classified as morbidly obese and lower levels of serum 25(OH)D can be seen in the morbidly obese patients secondary to a disturbance in tissue distribution, resulting from increased fat mass. It was demonstrated that the percentage of body fat is inversely related to serum levels of 25(OH)D in healthy women.39
Although the levels of VD were normal, the data in the present study show that they were not influenced by the dietary habits of the fishermen in the research since 31.75% of them did not eat eggs, only 31.75% ate fish (three times a week) and 95.27% were not taking supplements. VD can be obtained through food such as codfish liver oil, oily fish and eggs. However, these sources are scarce and humans depend mainly on the cutaneous production catalyzed by the UVB rays from the sun.
Sunlight is the most important source for VD because it stimulates the production of vitamin D3 in the skin and is dependent of, besides the factors already mentioned, the skin pigmentation, the clothing style and the use of sunscreen.40 Since the fishermen were exposed to the sun daily in 91.83% of the cases, working on average 21 to 28 hours per week and 32.19% of the time, this enables that 87.7% of those in the study have vitamin levels above 30ng/mL.
Other characteristics of the participants in this study, such as a low number (0.7%) of dark-skinned population (phototype IV) and the absence of the habit of using sunscreen and most of those researched (62.83%), could maybe have contributed to the low frequency of cases of vitamin D deficiency, since dark-skinned people have more difficulty with the transformation of 7-dehydrocholesterol into vitamin D, the serum concentration of 25(OH)D is lower and vitamin D deficiency is more common in patients using photoprotection.41,42
Serum levels of phosphorus, calcium and other factors can increase or reduce the renal production of 1.25 (OH) D. The 1,25(OH)D regulates its own synthesis and decreases the synthesis and secretion of PTH in parathyroid glands. Since most of the individuals had VD levels considered satisfactory by most authors, the finding of 100% of normal dosage of phosphorus and PTH and 98.34% of normal dosage of calcium was expected.
This high prevalence of elevated levels of vitamin D could have been responsible for the low incidence of NMSC in the fishermen once individuals with levels of 25 (OH) D of 32ng/mL seem to have a 40% lower risk of developing NMSC and, possibly, higher levels of 25 (OH) D can be a protective factor for the development of skin cancers. 43
Both the production of vitamin D and its implementation has demonstrated protective effects through mechanism involving the receptor vitamin D in many diseases and types of cancer, including skin cancer.44
VD produced in the skin can suppress the formation of epidermal tumors through VDR, binding 1.25(OH)D through the modulation of the activation or suppression of genes involved in the signaling of the processes that stop the cycle in G0/G1. This occurs via the inhibition of proliferation and stimulation of differentiation, immune regulation, and stimulation of DNA damage repair. Low levels of 1.25(OH)D could lead to the deregulation of these processes, promoting cell proliferation and inhibiting apoptosis.45–47
Besides, the vitamin D endogenously produced after exposure to UVB rays can have protective, antitumor, and photo adaptive activities against exposure to solar radiation after the initial exposure.48
ConclusionThere was a low prevalence of diagnosed cases of skin cancer among the fishermen when compared to the general population. In the cases diagnosed with skin cancer, the values found of SEI were higher than 10. A satisfactory rate of vitamin D, calcium, phosphorus, and parathyroid hormone was observed in the study population.
The study did not show a statistically proven relationship between sun exposure, vitamin D levels and clinical skin changes caused by solar exposure.
The fact that fishermen expose chronically to the sun, working for over 50 years exposed to the sun between 21 and 28 hours per week with no photoprotection contributed to a low frequency of vitamin D deficiency.
High levels of vitamin D could have been a protective factor against the development of skin cancer.